Клинический разбор в общей медицине №11 2024
Сандра Сьюзан Бину, Решма, Крипа Судит, Ганеш П. Сурахонн, Житто Томи
Кафедра фармацевтической практики, Фармацевтический колледж Бапуджи, Давангере, Индия
Цели. Оценить использование и эффективность кортикостероидов у пациентов, а также изучить схему назначения, демографические данные и клинические показатели, такие как лекарственное взаимодействие и нежелательные лекарственные реакции, связанные с введением кортикостероидов.
Методы. Проспективное поперечное исследование проводили на базе специализированной университетской клиники в течение 6 мес. Размер выборки составил 255 человек (125 пациентов пульмонологического профиля и 130 пациентов оториноларингологического профиля). Исследование было одобрено этическим комитетом Фармацевтического колледжа Бапуджи в Давангере. Были получены данные соответствовавших критериям включения в исследование лиц, которые приняли участие в опросе.
Результаты. Всего в исследование включили 255 человек (147 мужчин и 108 женщин), которым были назначены кортикостероиды. Возраст большинства пациентов составлял 61–70 лет. Наиболее часто рекомендуемым пациентам вариантом лечения была монотерапия. Наиболее часто применяемым кортикостероидом был гидрокортизон. Реже всего пациентам назначали мометазон. Кортикостероиды предпочитали вводить парентерально. В качестве двухкомпонентной терапии обычно применяли комбинацию дексаметазона и беклометазона. Формотерол и будесонид обычно использовали в сочетании с бронходилататорами. Головная боль и увеличение массы тела были самыми частыми побочными эффектами использования кортикостероидов. Пациентам пульмонологического профиля обычно назначали такие кортикостероиды, как гидрокортизон и будесонид.
Выводы. Исследование показало, что большинство пациентов хорошо реагировали на лечение кортикостероидами. Большая часть пациентов сочла кортикостероиды безопасными, в то время как у других пациентов имели место нежелательные лекарственные реакции. Побочные эффекты были зафиксированы у пациентов пульмонологического профиля, а у пациентов оториноларингологического профиля их не было.
Ключевые слова: кортикостероиды, стероиды, хроническая обструктивная болезнь легких, ХОБЛ, оториноларинголог, ЛОР, нежелательные лекарственные реакции, НЛР.
Для цитирования: Бину С.С., Решма, Судит K., Сурахонн Г.П., Томи Ж. Наблюдательное исследование по оценке использования, безопасности и эффективности кортикостероидов у пациентов оториноларингологического и пульмонологического отделений специализированной университетской клиники. Клинический разбор в общей медицине. 2024; 5 (11): 70–75. DOI: 10.47407/kr2024.5.11.00519
Drug utilization
Drug utilization, as defined by the World Health Organisation is the “marketing, distribution, prescription, and uses of drugs in the society, with special emphasis on the resulting medical, social and economic consequences” [5, 10]. Drug utilization trends serve as valuable exploratory tools for understanding the role of medications in medical practice. They are crucial for promoting the rational use of drugs and implementing effective interventions [5]. Rational drug use involves the concept of appropriateness, which must be evaluated in relation to treatment, concomitant diseases that may contraindicate or interfere with chosen therapy, and the patients other drug usage, including potential interactions [10].
Secondary objectives: To assess the patient's knowledge about the use of corticosteroids and to provide appropriate counselling to patients.
Hydrocortisone was the most frequently prescribed corticosteroids for the patients (29%) followed by Deflazacort and Fluticasone (17%). The least prescribed corticosteroids were Mometasone furoate (2%) (Table 1).
Parenteral route (30%) is the mostly prescribed route followed by oral (23%) for monotherapy.
Dexamethasone and beclomethasone were the most frequently used dual therapy (25.0%) (Table 2).
Parenteral and nasal (32%) routes were mostly prescribed in dual therapy followed by topical (25%). Budesonide with formoterol 98.6% was mostly prescribed combination therapy for the patients (Figure 2).
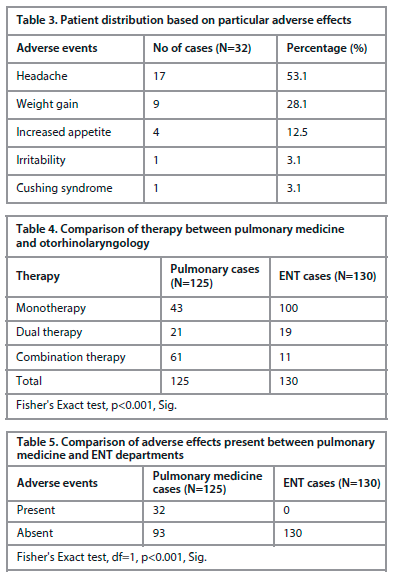 Out of 72 patients, 71 (98.6%) were given with nasal followed by oral l (1.4%) in combination therapy. Out of 255 patients, 32 (12.5%) had adverse events and 223 (87.5%) had no adverse events. Out of 32 patients, 14 (43,8%) used corticosteroid for 3months followed by 10 (31.3%) used for 12 months and 7 (21.9%) used for 6 months and 1 (3.1%) used for 24 months. Out of 32 patients, headache was most identified adverse event in 17 (53.1%) patients followed by weight gain was seen in 9 (28.1%) patients and 4 (12.5%) patients presented with increased appetite, cushing syndrome and irritability was identified in 1 (3.1%) patient (Table 3).
Out of 72 patients, 71 (98.6%) were given with nasal followed by oral l (1.4%) in combination therapy. Out of 255 patients, 32 (12.5%) had adverse events and 223 (87.5%) had no adverse events. Out of 32 patients, 14 (43,8%) used corticosteroid for 3months followed by 10 (31.3%) used for 12 months and 7 (21.9%) used for 6 months and 1 (3.1%) used for 24 months. Out of 32 patients, headache was most identified adverse event in 17 (53.1%) patients followed by weight gain was seen in 9 (28.1%) patients and 4 (12.5%) patients presented with increased appetite, cushing syndrome and irritability was identified in 1 (3.1%) patient (Table 3).
Out of 143 patients, those prescribed with Hydrocortisone 15 patients presented adverse events and those prescribed with Budesonide and Methylprednisolone 2 patients presented adverse events. Out of 49 patients, those prescribed with hydrocortisone with budesonide and budesonide with methylprednisolone 2 presented with adverse events those prescribed with hydrocortisone with methylprednisolone 1 presented with adverse event and those given with hydrocortisone with fluticasone and methylprednisolone with deflazacort 1 presented with adverse event. By using Fisher exact test, the P value was found to be <0.05 which was significant. Out of 72 patients, those prescribed with formoterol + budesonide combination 6 presented with adverse event. Out of 255 patients, only monotherapy was given to 43 patients from pulmonary medicine and 100 patients from ENT.
Dual therapy was given to 21 patients from pulmonary medicine and 19 patients from ENT. Combination therapy was given to 61 patients from pulmonary medicine and 11 from ENT (Table 4).
32 pulmonary cases were presented with adverse effects and no effects were seen in ENT cases (Table 5).
Hydrocortisone is the mostly prescribed corticosteroid among pulmonary medicine patients. Deflazacort and fluticasone are the mostly prescribed among ENT patients. Hydrocortisone and budesonide are the corticosteroids mostly prescribed for the Pulmonary medicine patients. Dexamethasone and beclomethasone are the drugs mostly prescribed for ENT patients. Formoterol + budesonide is the most commonly prescribed combination therapy among pulmonary and ENT patients.
In the present study age wise distribution, 34 (13.3%) was prescribed with corticosteroid in age group less than 10 years, 16 (6.3%) patients in 11–20 years, 22 (8.6%) in 21–30 years, 30 (11.8%) in 31–40 years, 28 (11%) in 41–50 years, 42 (16.5%) in 51–60 years, 46 (18%) patients from age group of 61–70 years, 29 (11.4%) in 71–80 years and 8 (3.1%) in 81–90 years prescribed with corticosteroids. The mean age of patients was 45.33±23.53. In this the prescribing of corticosteroids were more among age group of 61–70 years. This was comparable with the studies of Makbul Hussain Chowdhury et al. [5] who found that mean age of patients was 46.66±15.23.
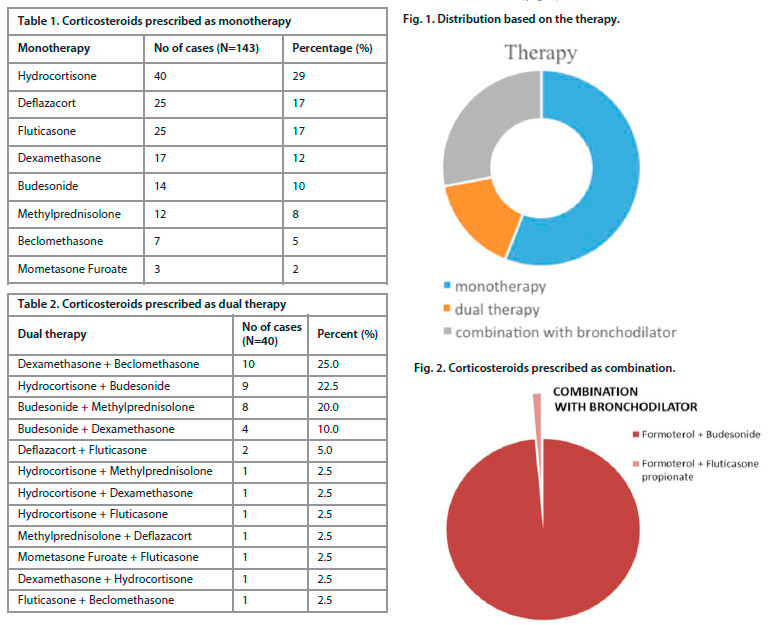
In our study out of 255 patients, 143 (56%) were given with monotherapy, 40 (16%) were given with dual therapy and 72 (28%) were given with combination of corticosteroid with bronchodilator. In the study conducted by Syeda Masarrath Unissa et al. [6] the mostly prescribed corticosteroid was Budesonide (31.75%) and the least prescribed corticosteroid was Methylprednisolone (5.56%). In our study, the monotherapy of corticosteroid prescribed to 143 patients include 40 (29%) Hydrocortisone, 14 (10%) Budesonide, 12 (8%) Methylprednisolone, 3 (2%) Mometasone furoate, 17 (12%) Dexamethasone, 25 (17%) Deflazacort,
25 (17%) Fluticasone and 7 (5%) Beclomethasone among these the mostly prescribed corticosteroid was Hydrocortisone with the percentage of 29% and the least prescribed corticosteroid was Mometasone furoate with the percentage of 2%.
In the study conducted by Vishwanath Gouda et al. [11] the mostly used dual therapy of corticosteroid was Budesonide + Hydrocortisone (6.68%). In our study, out of 40 patients, 10 (25%) Dexamethasone + Beclomethasone and 9 (22.5%) Hydrocortisones + Budesonide was mostly used dual therapy of corticosteroid.
In the present study we included 72 patients who were prescribed with the combination of corticosteroid with bronchodilator and most preferred combination include 71 (98.6%) patients were given with Formoterol + Budesonide and 1 (1.4%) patient were given with Formoterol + Fluticasone propionate. Since, this drug is more prone to adverse drug reactions. In the study conducted by Makbul Hussain Chowdhury et al. [5] found 34 adverse drug reaction among 200 patients. In our study out of 255 patients, 32 (12.5%) patients were found to have adverse drug reaction and 223 (87.5%) patients with no adverse drug reaction. In our study out 32 adverse drug reaction patients, the corticosteroid duration of use was categorised based on months, mostly it was given for 3 months 14 (43.8%), 6 months 7 (21.9%), 12 months 10 (31.3%) and 24 months 1 (3.1%).
In the study conducted by Shazma Imam et al. [19] identified 3 adverse drug reaction out of which 2 (67%) were headache and 1 (33%) was facial puffiness. In our study out of 32 patients most identified adverse drug reaction were 17 (53.1%) headache, 9 (28.1%) weight gain, 1 (3.1%) irritability, 4 (12.5%) increased appetite and 1 (3.1%) Cushing syndrome. Out of 143 monotherapies prescribed 15 patients showed adverse drug reaction due to Hydrocortisone, 2 patients due to Budesonide and 2 patients due to Methylprednisolone.
This study also focused on corticosteroid use among pulmonary medicine and otorhinolaryngology departments, hence the comparison of the result can be done among these departments. Out of 125 patients from pulmonary medicine 43 prescribed with monotherapy, 21 prescribed with dual therapy and 61 prescribed with combination of corticosteroid with bronchodilator. Out of 130 patients from otorhinolaryngology 100 prescribed with monotherapy, 19 prescribed with dual therapy and 11 prescribed with combination of corticosteroid with bronchodilator. Monotherapy were mostly prescribed in ENT compare to pulmonary medicine and combination of corticosteroid with bronchodilator were mostly prescribed in pulmonary medicine compare to ENT.
In our study, 32 patients were identified with adverse drug reaction associated with corticosteroid use and all the 32 patients were from pulmonary medicine and no patients were identified with adverse drug reaction from ENT. In our study, out of 143 monotherapies, hydrocortisone was mostly prescribed among pulmonary medicine and Deflazacort and Fluticasone was mostly prescribed among ENT. Out of 40 dual therapies, Hydrocortisone plus Budesonide, Budesonide plus Methylprednisolone was mostly prescribed among pulmonary medicine and Dexamethasone plus Beclomethasone was prescribed among ENT. Out of 72 combinations of corticosteroid with bronchodilator therapy, Formoterol plus Budesonide was used among both the departments.
Drug utilization, marketing, distribution, prescription writing, and drug use in the society are all considered forms of drug utilization according to the World Health Organization. Particular attention is paid to the economic, social, and medical repercussions of these activities. Trends in drug use serve as effective, exploratory instruments for determining the place of drugs in medicine. It goes without saying that encouraging interventions and responsible drug use are important.
The medication adherence pattern has significantly improved after pharmacist intervention through counselling and drug information leaflets. The continuous identification and resolution by the addition of a clinical pharmacist through their knowledge and expertise can enhance the pharmaceutical care which help to reduce the occurrence of drug-related problems and improve barriers for medication adherence.
Limitations
During the phone call follow-up, a patient fails to identify the adverse effect. Difficulty to identify the drug interaction based on route of administration. Due to time constraints, some people refuse to complete the ADR questionnaire. Errors and lack of clinical details where some of this study's other weaknesses.
Declaration by authors
Source of funding. This publication was prepared without any external funding.
Authors contribution. Sandra Susan Binu: data collection, investigations, writing – original draft. Reshma: data collection, investigations, writing – original draft. Kripa Sujith: data collection, investigations, writing – original draft. Ganesh P. Surahonne: data collection, investigations, writing – original draft. Jitto Tomy: conceptualization, methodology, formal analysis, supervision, writing – review and editing.
Acknowledgments. We want to thank all the faculties of the Department of Pharmacy Practice, Bapuji Pharmacy College and the Department of Pulmonary medicine and Department of ENT, S.S. Institute of Medical Sciences and Research Centre, Davangere, for their valuable suggestions and advice. We would also like to express our sincere gratitude to Bapuji Pharmacy College and SSIMS & RC Hospital for providing the necessary facilities to conduct the research.
Conflict of interest. The authors declare no conflict of interest.
Information about the authors
Sandra Susan Binu – Pharm. D. Intern, Department of Pharmacy Practice, Bapuji Pharmacy College, Rajiv Gandhi University of Health Sciences. ORCID: 0009-0007-4149-0359
Reshma – Pharm. D. Intern, Department of Pharmacy Practice, Bapuji Pharmacy College, Rajiv Gandhi University of Health Sciences. ORCID: 0009-0004-8012-3816
Kripa Sujith – Pharm. D. Intern, Department of Pharmacy Practice, Bapuji Pharmacy College, Rajiv Gandhi University of Health Sciences. ORCID: 0009-0000-4354-7717
Ganesh P. Surahonne – Pharm. D. Intern, Department of Pharmacy Practice, Bapuji Pharmacy College, Rajiv Gandhi University of Health Sciences. ORCID: 0009-0009-4339-3581
Dr Jitto Tomy – Assistant Professor, Department of Pharmacy Practice, Bapuji Pharmacy College, Rajiv Gandhi University of Health Sciences. ORCID: 0009-0002-9618-6753
Received: 15.08.2024
Revised: 21.08.2024
Accepted: 28.08.2024
Клинический разбор в общей медицине №11 2024
An observational study on utilization, safety and efficacy of corticosteroids in otorhinolaryngology and pulmonary medicine patients in a tertiary care teaching hospital
Номера страниц в выпуске:70-75
Abstract
Introduction. Corticosteroids, commonly referred to as steroids, are anti-inflammatory medications primarily utilized to decrease inflammation and suppress the immune system. Drug utilization plays an important role in medical practice for providing rationality in prescribing medications.
Objectives. To evaluate the utilization and efficacy of corticosteroids in patients and to assess the prescribing pattern, demographics, and clinical variables such as drug interaction, and adverse drug reactions associated with corticosteroid administration.
Methodology. A prospective Cross-sectional study was conducted in a tertiary care teaching hospital for a period of 6 months. The sample size of the study was 255 (125-pulmonary medicine and 130-ENT). The study obtained ethical approval from the Institutional Ethics Committee at Bapuji Pharmacy College in Davangere. Data were collected from the subjects who participated in the survey who met inclusion criteria.
Results. The study included 255 participants in total, 147 of whom were male and 108 of whom were female and had been prescribed with corticosteroids. Most of the patients were in the 61–70 age range. The most often recommended form of treatment for the individuals was monotherapy. The most administered corticosteroids for the patients were Hydrocortisone. Patients are prescribed Mometasone as a corticosteroid with the least frequency. To provide corticosteroids most preferred route of administration was parenteral. A combination of Dexamethasone and Beclomethasone was commonly administered in dual therapy. Formoterol plus budesonide was commonly used in conjunction with bronchodilators. Headache and weight gain were the most frequent side effects of using corticosteroids. Patients in pulmonary medicine are typically prescribed hydrocortisone and budesonide as corticosteroids.
Conclusion. According to this study, the majority of patients responded well to corticosteroid treatment. Most patients found corticosteroids to be safe, while some experienced adverse drug reactions (ADRs). Adverse effects were reported in pulmonary instances, however no adverse effects were observed in ENT patients.
Keywords: corticosteroids, steroids, chronic obstructive pulmonary disease, COPD, ear nose throat, ENT, adverse drug reactions, ADRs.
For citation: Binu S.S., Reshma, Sujith K., Surahonne G.P., Tomy J. An observational study on utilization, safety and efficacy of corticosteroids in otorhinolaryngology and pulmonary medicine patients in a tertiary care teaching hospital. Clinical review for general practice. 2024; 5 (11): 70–75 (In Russ.). DOI: 10.47407/kr2024.5.11.00519
Introduction. Corticosteroids, commonly referred to as steroids, are anti-inflammatory medications primarily utilized to decrease inflammation and suppress the immune system. Drug utilization plays an important role in medical practice for providing rationality in prescribing medications.
Objectives. To evaluate the utilization and efficacy of corticosteroids in patients and to assess the prescribing pattern, demographics, and clinical variables such as drug interaction, and adverse drug reactions associated with corticosteroid administration.
Methodology. A prospective Cross-sectional study was conducted in a tertiary care teaching hospital for a period of 6 months. The sample size of the study was 255 (125-pulmonary medicine and 130-ENT). The study obtained ethical approval from the Institutional Ethics Committee at Bapuji Pharmacy College in Davangere. Data were collected from the subjects who participated in the survey who met inclusion criteria.
Results. The study included 255 participants in total, 147 of whom were male and 108 of whom were female and had been prescribed with corticosteroids. Most of the patients were in the 61–70 age range. The most often recommended form of treatment for the individuals was monotherapy. The most administered corticosteroids for the patients were Hydrocortisone. Patients are prescribed Mometasone as a corticosteroid with the least frequency. To provide corticosteroids most preferred route of administration was parenteral. A combination of Dexamethasone and Beclomethasone was commonly administered in dual therapy. Formoterol plus budesonide was commonly used in conjunction with bronchodilators. Headache and weight gain were the most frequent side effects of using corticosteroids. Patients in pulmonary medicine are typically prescribed hydrocortisone and budesonide as corticosteroids.
Conclusion. According to this study, the majority of patients responded well to corticosteroid treatment. Most patients found corticosteroids to be safe, while some experienced adverse drug reactions (ADRs). Adverse effects were reported in pulmonary instances, however no adverse effects were observed in ENT patients.
Keywords: corticosteroids, steroids, chronic obstructive pulmonary disease, COPD, ear nose throat, ENT, adverse drug reactions, ADRs.
For citation: Binu S.S., Reshma, Sujith K., Surahonne G.P., Tomy J. An observational study on utilization, safety and efficacy of corticosteroids in otorhinolaryngology and pulmonary medicine patients in a tertiary care teaching hospital. Clinical review for general practice. 2024; 5 (11): 70–75 (In Russ.). DOI: 10.47407/kr2024.5.11.00519
Наблюдательное исследование по оценке использования, безопасности и эффективности кортикостероидов у пациентов оториноларингологического и пульмонологического отделений специализированной университетской клиники
Сандра Сьюзан Бину, Решма, Крипа Судит, Ганеш П. Сурахонн, Житто Томи
Кафедра фармацевтической практики, Фармацевтический колледж Бапуджи, Давангере, Индия
Аннотация
Введение. Кортикостероиды, обычно называемые стероидами, – это противовоспалительные средства, используемые в первую очередь для уменьшения воспаления и подавления иммунной системы. Использование лекарственных средств играет важную роль в медицинской практике, обеспечивая рациональность назначения лекарств.Цели. Оценить использование и эффективность кортикостероидов у пациентов, а также изучить схему назначения, демографические данные и клинические показатели, такие как лекарственное взаимодействие и нежелательные лекарственные реакции, связанные с введением кортикостероидов.
Методы. Проспективное поперечное исследование проводили на базе специализированной университетской клиники в течение 6 мес. Размер выборки составил 255 человек (125 пациентов пульмонологического профиля и 130 пациентов оториноларингологического профиля). Исследование было одобрено этическим комитетом Фармацевтического колледжа Бапуджи в Давангере. Были получены данные соответствовавших критериям включения в исследование лиц, которые приняли участие в опросе.
Результаты. Всего в исследование включили 255 человек (147 мужчин и 108 женщин), которым были назначены кортикостероиды. Возраст большинства пациентов составлял 61–70 лет. Наиболее часто рекомендуемым пациентам вариантом лечения была монотерапия. Наиболее часто применяемым кортикостероидом был гидрокортизон. Реже всего пациентам назначали мометазон. Кортикостероиды предпочитали вводить парентерально. В качестве двухкомпонентной терапии обычно применяли комбинацию дексаметазона и беклометазона. Формотерол и будесонид обычно использовали в сочетании с бронходилататорами. Головная боль и увеличение массы тела были самыми частыми побочными эффектами использования кортикостероидов. Пациентам пульмонологического профиля обычно назначали такие кортикостероиды, как гидрокортизон и будесонид.
Выводы. Исследование показало, что большинство пациентов хорошо реагировали на лечение кортикостероидами. Большая часть пациентов сочла кортикостероиды безопасными, в то время как у других пациентов имели место нежелательные лекарственные реакции. Побочные эффекты были зафиксированы у пациентов пульмонологического профиля, а у пациентов оториноларингологического профиля их не было.
Ключевые слова: кортикостероиды, стероиды, хроническая обструктивная болезнь легких, ХОБЛ, оториноларинголог, ЛОР, нежелательные лекарственные реакции, НЛР.
Для цитирования: Бину С.С., Решма, Судит K., Сурахонн Г.П., Томи Ж. Наблюдательное исследование по оценке использования, безопасности и эффективности кортикостероидов у пациентов оториноларингологического и пульмонологического отделений специализированной университетской клиники. Клинический разбор в общей медицине. 2024; 5 (11): 70–75. DOI: 10.47407/kr2024.5.11.00519
Introduction
Steroids, commonly known as corticosteroids, are anti-inflammatory medications prescribed for a range of conditions [1]. These drugs are synthetic analogs of hormones that are naturally produced by the adrenal glands, which are small glands situated above the kidneys. The major purposes of corticosteroids are immune system suppression and inflammation reduction [1]. Additionally, corticosteroids may be used to replace specific hormones that the body is unable to manufacture on its own, like in the case of Addison's disease patients [1]. Corticosteroids have demonstrated remarkable effectiveness in treating both acute and chronic inflammatory conditions; cortisol was first isolated in 1950 [5]. Oral corticosteroids (OCS) are used with caution despite their therapeutic efficacy because of potentially serious side effects, including osteoporosis, bone fractures, and increased susceptibility to infections, hyperglycaemia, and obesity [5]. To treat a variety of disorders, glucocorticoids are frequently utilized as effective immunosuppressive and anti-inflammatory medications [4]. They do, however, also come with a multitude of adverse effects. In general, corticosteroids are referred to as "steroids"; they significantly reduce symptoms and provide notable effects in a variety of illnesses. Healthcare professionals commonly prescribe corticosteroids due to their potent anti-inflammatory and immune-modulating properties [4]. Corticosteroids are most commonly prescribed to patients with respiratory diseases like asthma or chronic obstructive pulmonary disease (COPD) [4]. The method of administration for these medications varies based on several factors, with the specific condition being treated being the most significant.Otorhinolaryngology
This medical specialty focuses on diagnosing and treating conditions related to the ears, nose, and throat. Professionals in this field are trained in both surgery and medical practices [10]. This category includes mostly inflammatory conditions of nose, ear, and throat. In this condition physicians are generally prescribed with the anti-inflammatory, that is, corticosteroids [10]. The study encompasses diseases affecting the outer ear, middle ear and mastoid, and inner ear, and adjacent structures including the facial nerve and lateral skull base.Pulmonary medicine
Pulmonary medicine is a comprehensive medical speciality that focuses primarily on diseases affecting the lungs, including asthma, pneumonia, allergies, COPD, lung cancers and infectious lung disease. Additionally, it encompasses fields such as critical care and sleep medicine [1].Drug utilization
Drug utilization, as defined by the World Health Organisation is the “marketing, distribution, prescription, and uses of drugs in the society, with special emphasis on the resulting medical, social and economic consequences” [5, 10]. Drug utilization trends serve as valuable exploratory tools for understanding the role of medications in medical practice. They are crucial for promoting the rational use of drugs and implementing effective interventions [5]. Rational drug use involves the concept of appropriateness, which must be evaluated in relation to treatment, concomitant diseases that may contraindicate or interfere with chosen therapy, and the patients other drug usage, including potential interactions [10].
Safety and efficacy
Safety is defined in terms of risk and efficacy in terms of a benefit. Both are discussed in terms of probability and magnitude of benefit and harm [15]. A drug is effective if it has ‘the effect it purports or is represented to have under the conditions of use prescribed, recommended, or suggested in the proposed labelling thereof.’ Safety represents “a value judgement of the acceptability of risk.” Risk can be defined as “a measure of the probability and severity of harm to human health” [15].Objectives
Primary objectives: To evaluate the utilization and efficacy of corticosteroids in patients and to assess the prescribing pattern, demographics, and clinical variables such as adverse drug reactions associated with corticosteroid administration.Secondary objectives: To assess the patient's knowledge about the use of corticosteroids and to provide appropriate counselling to patients.
Materials & methods
A prospective cross-sectional descriptive study was conducted at Shamanur Shivashankarappa Institute of Medical Sciences and Research Centre (SSIMS & RC) in Davangere over a period of six months. The study included 255 patients from both the ENT and Pulmonary Medicine departments, with the inclusion criteria of patients aged one and above who received any category of corticosteroid therapy in these departments, regardless of sex, and included both inpatient and outpatient participants. Exclusion criteria comprised critically ill patients, pregnant and lactating women, HIV and cancer chemotherapy patients, unwilling participants, and those with mental disabilities. Data were collected from treatment charts, patient case notes, Lexicomp, and lab investigation reports. Materials such as a data collection form, drug information leaflets, Lexicomp for identifying drug interactions, and a corticosteroid ADR questionnaire were used in the study. Ethical clearance was obtained from the Institutional Ethical Committee in Davangere. The study enrolled patients prescribed with corticosteroids and caretakers of pediatric patients from both departments, collecting demographic details such as comorbidities, age, sex, and educational status, and assessing ADRs caused by corticosteroids using a self-prepared questionnaire. Data were represented graphically and analysed using Fisher's exact test.Results
A Prospective cross-sectional descriptive study was conducted on 255 patients from both the Pulmonary medicine and otorhinolaryngology departments. We analysed the drug utilization pattern, safety, and efficacy of corticosteroids prescribed for the same. A total of 255 patients were included in the study. Out of which, 125 (49%) are from Pulmonary medicine and 130 (51%) are from the otorhinolaryngology department. The highest number of patients prescribed with corticosteroids was found between the age group of 61 to 70 years (18%) and the lowest between 81 – 90 (8%). In our study, 147 (57.6%) patients were men and 108 (42.4%) were women. In the study population, 175 (68.6%) were not found to have any additive habits, 59(19.7%) patients were smokers, 40(13.3%) patients were alcoholics and 22 (7.3%) were tobacco chewers. Out of 255 patients, 143 (56%) patients were prescribed with monotherapy, 40(16%) patients were prescribed with dual therapy, 21(8%) patients were given with combination of corticosteroid with bronchodilator (Figure 1).Hydrocortisone was the most frequently prescribed corticosteroids for the patients (29%) followed by Deflazacort and Fluticasone (17%). The least prescribed corticosteroids were Mometasone furoate (2%) (Table 1).
Parenteral route (30%) is the mostly prescribed route followed by oral (23%) for monotherapy.
Dexamethasone and beclomethasone were the most frequently used dual therapy (25.0%) (Table 2).
Parenteral and nasal (32%) routes were mostly prescribed in dual therapy followed by topical (25%). Budesonide with formoterol 98.6% was mostly prescribed combination therapy for the patients (Figure 2).
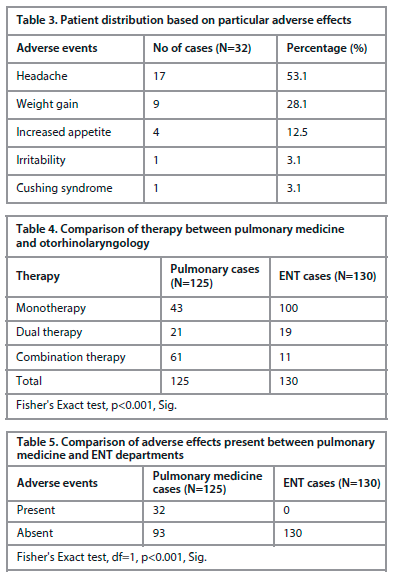 Out of 72 patients, 71 (98.6%) were given with nasal followed by oral l (1.4%) in combination therapy. Out of 255 patients, 32 (12.5%) had adverse events and 223 (87.5%) had no adverse events. Out of 32 patients, 14 (43,8%) used corticosteroid for 3months followed by 10 (31.3%) used for 12 months and 7 (21.9%) used for 6 months and 1 (3.1%) used for 24 months. Out of 32 patients, headache was most identified adverse event in 17 (53.1%) patients followed by weight gain was seen in 9 (28.1%) patients and 4 (12.5%) patients presented with increased appetite, cushing syndrome and irritability was identified in 1 (3.1%) patient (Table 3).
Out of 72 patients, 71 (98.6%) were given with nasal followed by oral l (1.4%) in combination therapy. Out of 255 patients, 32 (12.5%) had adverse events and 223 (87.5%) had no adverse events. Out of 32 patients, 14 (43,8%) used corticosteroid for 3months followed by 10 (31.3%) used for 12 months and 7 (21.9%) used for 6 months and 1 (3.1%) used for 24 months. Out of 32 patients, headache was most identified adverse event in 17 (53.1%) patients followed by weight gain was seen in 9 (28.1%) patients and 4 (12.5%) patients presented with increased appetite, cushing syndrome and irritability was identified in 1 (3.1%) patient (Table 3).Out of 143 patients, those prescribed with Hydrocortisone 15 patients presented adverse events and those prescribed with Budesonide and Methylprednisolone 2 patients presented adverse events. Out of 49 patients, those prescribed with hydrocortisone with budesonide and budesonide with methylprednisolone 2 presented with adverse events those prescribed with hydrocortisone with methylprednisolone 1 presented with adverse event and those given with hydrocortisone with fluticasone and methylprednisolone with deflazacort 1 presented with adverse event. By using Fisher exact test, the P value was found to be <0.05 which was significant. Out of 72 patients, those prescribed with formoterol + budesonide combination 6 presented with adverse event. Out of 255 patients, only monotherapy was given to 43 patients from pulmonary medicine and 100 patients from ENT.
Dual therapy was given to 21 patients from pulmonary medicine and 19 patients from ENT. Combination therapy was given to 61 patients from pulmonary medicine and 11 from ENT (Table 4).
32 pulmonary cases were presented with adverse effects and no effects were seen in ENT cases (Table 5).
Hydrocortisone is the mostly prescribed corticosteroid among pulmonary medicine patients. Deflazacort and fluticasone are the mostly prescribed among ENT patients. Hydrocortisone and budesonide are the corticosteroids mostly prescribed for the Pulmonary medicine patients. Dexamethasone and beclomethasone are the drugs mostly prescribed for ENT patients. Formoterol + budesonide is the most commonly prescribed combination therapy among pulmonary and ENT patients.
Discussion
The present study was conducted among 255 patients in South India for 6-month period. The aim of the study was to evaluate utilization, safety, and efficacy of corticosteroids in patients and to assess the prescribing pattern, demographics, and clinical variables such as drug interaction, adverse drug reactions associated with corticosteroid administration, to assess the patient knowledge about the use of corticosteroids and to provide appropriate counselling to patients. In this study out of 255 patients there were 125 from pulmonary medicine and 130 from otorhinolaryngology department. Corticosteroids being widely used powerful anti-inflammatory and immunosuppressive agents and have become one of the most prescribed drugs in acute and chronic inflammatory diseases. Corticosteroids though are lifesaving drugs; it produces adverse reactions which may be mild or life threatening. This study included 255 patients out of which 147 (57.6%) were male and 108 (42.4%) were female where males was more compared to females as similar in study conducted by Mani Pandey et al. [12], however in the study conducted by Makbul Hussain Chowdhury et al. [5] the female patients was more compare to male patients.In the present study age wise distribution, 34 (13.3%) was prescribed with corticosteroid in age group less than 10 years, 16 (6.3%) patients in 11–20 years, 22 (8.6%) in 21–30 years, 30 (11.8%) in 31–40 years, 28 (11%) in 41–50 years, 42 (16.5%) in 51–60 years, 46 (18%) patients from age group of 61–70 years, 29 (11.4%) in 71–80 years and 8 (3.1%) in 81–90 years prescribed with corticosteroids. The mean age of patients was 45.33±23.53. In this the prescribing of corticosteroids were more among age group of 61–70 years. This was comparable with the studies of Makbul Hussain Chowdhury et al. [5] who found that mean age of patients was 46.66±15.23.
In our study out of 255 patients, 143 (56%) were given with monotherapy, 40 (16%) were given with dual therapy and 72 (28%) were given with combination of corticosteroid with bronchodilator. In the study conducted by Syeda Masarrath Unissa et al. [6] the mostly prescribed corticosteroid was Budesonide (31.75%) and the least prescribed corticosteroid was Methylprednisolone (5.56%). In our study, the monotherapy of corticosteroid prescribed to 143 patients include 40 (29%) Hydrocortisone, 14 (10%) Budesonide, 12 (8%) Methylprednisolone, 3 (2%) Mometasone furoate, 17 (12%) Dexamethasone, 25 (17%) Deflazacort,
25 (17%) Fluticasone and 7 (5%) Beclomethasone among these the mostly prescribed corticosteroid was Hydrocortisone with the percentage of 29% and the least prescribed corticosteroid was Mometasone furoate with the percentage of 2%.
In the study conducted by Vishwanath Gouda et al. [11] the mostly used dual therapy of corticosteroid was Budesonide + Hydrocortisone (6.68%). In our study, out of 40 patients, 10 (25%) Dexamethasone + Beclomethasone and 9 (22.5%) Hydrocortisones + Budesonide was mostly used dual therapy of corticosteroid.
In the present study we included 72 patients who were prescribed with the combination of corticosteroid with bronchodilator and most preferred combination include 71 (98.6%) patients were given with Formoterol + Budesonide and 1 (1.4%) patient were given with Formoterol + Fluticasone propionate. Since, this drug is more prone to adverse drug reactions. In the study conducted by Makbul Hussain Chowdhury et al. [5] found 34 adverse drug reaction among 200 patients. In our study out of 255 patients, 32 (12.5%) patients were found to have adverse drug reaction and 223 (87.5%) patients with no adverse drug reaction. In our study out 32 adverse drug reaction patients, the corticosteroid duration of use was categorised based on months, mostly it was given for 3 months 14 (43.8%), 6 months 7 (21.9%), 12 months 10 (31.3%) and 24 months 1 (3.1%).
In the study conducted by Shazma Imam et al. [19] identified 3 adverse drug reaction out of which 2 (67%) were headache and 1 (33%) was facial puffiness. In our study out of 32 patients most identified adverse drug reaction were 17 (53.1%) headache, 9 (28.1%) weight gain, 1 (3.1%) irritability, 4 (12.5%) increased appetite and 1 (3.1%) Cushing syndrome. Out of 143 monotherapies prescribed 15 patients showed adverse drug reaction due to Hydrocortisone, 2 patients due to Budesonide and 2 patients due to Methylprednisolone.
This study also focused on corticosteroid use among pulmonary medicine and otorhinolaryngology departments, hence the comparison of the result can be done among these departments. Out of 125 patients from pulmonary medicine 43 prescribed with monotherapy, 21 prescribed with dual therapy and 61 prescribed with combination of corticosteroid with bronchodilator. Out of 130 patients from otorhinolaryngology 100 prescribed with monotherapy, 19 prescribed with dual therapy and 11 prescribed with combination of corticosteroid with bronchodilator. Monotherapy were mostly prescribed in ENT compare to pulmonary medicine and combination of corticosteroid with bronchodilator were mostly prescribed in pulmonary medicine compare to ENT.
In our study, 32 patients were identified with adverse drug reaction associated with corticosteroid use and all the 32 patients were from pulmonary medicine and no patients were identified with adverse drug reaction from ENT. In our study, out of 143 monotherapies, hydrocortisone was mostly prescribed among pulmonary medicine and Deflazacort and Fluticasone was mostly prescribed among ENT. Out of 40 dual therapies, Hydrocortisone plus Budesonide, Budesonide plus Methylprednisolone was mostly prescribed among pulmonary medicine and Dexamethasone plus Beclomethasone was prescribed among ENT. Out of 72 combinations of corticosteroid with bronchodilator therapy, Formoterol plus Budesonide was used among both the departments.
Conclusion
The outcome of this study has emphasized the drug utilization pattern, safety, and efficacy of corticosteroid among otorhinolaryngology and pulmonary medicine patients. In the study, the majority of patients responded well to the treatment. Most patients found corticosteroid to be safe for daily use while some experienced adverse drug reactions. However, no reactions were seen in ENT patients.Drug utilization, marketing, distribution, prescription writing, and drug use in the society are all considered forms of drug utilization according to the World Health Organization. Particular attention is paid to the economic, social, and medical repercussions of these activities. Trends in drug use serve as effective, exploratory instruments for determining the place of drugs in medicine. It goes without saying that encouraging interventions and responsible drug use are important.
The medication adherence pattern has significantly improved after pharmacist intervention through counselling and drug information leaflets. The continuous identification and resolution by the addition of a clinical pharmacist through their knowledge and expertise can enhance the pharmaceutical care which help to reduce the occurrence of drug-related problems and improve barriers for medication adherence.
Limitations
During the phone call follow-up, a patient fails to identify the adverse effect. Difficulty to identify the drug interaction based on route of administration. Due to time constraints, some people refuse to complete the ADR questionnaire. Errors and lack of clinical details where some of this study's other weaknesses.
Declaration by authors
Source of funding. This publication was prepared without any external funding.
Authors contribution. Sandra Susan Binu: data collection, investigations, writing – original draft. Reshma: data collection, investigations, writing – original draft. Kripa Sujith: data collection, investigations, writing – original draft. Ganesh P. Surahonne: data collection, investigations, writing – original draft. Jitto Tomy: conceptualization, methodology, formal analysis, supervision, writing – review and editing.
Acknowledgments. We want to thank all the faculties of the Department of Pharmacy Practice, Bapuji Pharmacy College and the Department of Pulmonary medicine and Department of ENT, S.S. Institute of Medical Sciences and Research Centre, Davangere, for their valuable suggestions and advice. We would also like to express our sincere gratitude to Bapuji Pharmacy College and SSIMS & RC Hospital for providing the necessary facilities to conduct the research.
Conflict of interest. The authors declare no conflict of interest.
Information about the authors
Sandra Susan Binu – Pharm. D. Intern, Department of Pharmacy Practice, Bapuji Pharmacy College, Rajiv Gandhi University of Health Sciences. ORCID: 0009-0007-4149-0359
Reshma – Pharm. D. Intern, Department of Pharmacy Practice, Bapuji Pharmacy College, Rajiv Gandhi University of Health Sciences. ORCID: 0009-0004-8012-3816
Kripa Sujith – Pharm. D. Intern, Department of Pharmacy Practice, Bapuji Pharmacy College, Rajiv Gandhi University of Health Sciences. ORCID: 0009-0000-4354-7717
Ganesh P. Surahonne – Pharm. D. Intern, Department of Pharmacy Practice, Bapuji Pharmacy College, Rajiv Gandhi University of Health Sciences. ORCID: 0009-0009-4339-3581
Dr Jitto Tomy – Assistant Professor, Department of Pharmacy Practice, Bapuji Pharmacy College, Rajiv Gandhi University of Health Sciences. ORCID: 0009-0002-9618-6753
Received: 15.08.2024
Revised: 21.08.2024
Accepted: 28.08.2024
Список исп. литературыСкрыть список1. Liu D, Ahmet A, Ward L et al. A practical guide to the monitoring and management of the complications of systemic corticosteroid therapy. Allergy Asthma Clin Immunol 2013;9(1):30.
2. Coutinho AE, Chapman KE. The anti-inflammatory and immunosuppressive effects of glucocorticoids, recent developments and mechanistic insights. Mol Cell Endocrinol 2011;335(1):2-13.
3. Thakur PK, Majid A, Shramik M et al. A Prospective Study on Drug Utilization Evaluation of Corticosteroids among Out-Patients of Teaching Hospital Project. IJPTP 2015;6(4):2630-4.
4. Beg MA, Dutta SB, Bawa S et al. Prescribing trends in respiratory tract infections in a tertiary care teaching hospital. Int J Res Med Sci 2017;(5):2588-1.
5. Chowdhury MH, Shravya K, Prasad M et al. Evaluation of Corticosteroid Utilization Pattern in the Various Departments of a Tertiary Care Teaching Hospital, Khammam. Saudi J Med Pharm Sci 2019;5(12):1094.
6. Unissa SM, Kareem S, Ahmed SF et al. A Prospective Observational Studies on Drug Utilization Evaluation and Rational Use of Corticosteroids in Tertiary Care Hospital. J Drug Delivery Ther 2020;10(5-s):119.
7. Streeten DH. Corticosteroid therapy. I. Pharmacological properties and principles of corticosteroid use. JAMA 1975;232(9):944-7.
8. Ericson-Neilsen W, Kaye AD. Steroids: pharmacology, complications, and practice delivery issues. Ochsner J 2014;14(2):203-7.
9. Da Silva JA, Jacobs JW, Kirwan JR et al. Safety of low dose glucocorticoid treatment in rheumatoid arthritis: published evidence and prospective trial data. Ann Rheum Dis 2006;65(3):285-3.
10. Vijay R, Atray M. Drug utilization pattern in ENT outpatient department in tertiacare teaching hospital in Southern Rajasthan. Natl J Physiol Pharm Pharmacol 2022;(2).
11. Gouda V, Shastry CS, Mateti UV et al. Study on Steroid Utilization Patterns in General Medicine Department. Research J Pharm Tech 2019;12(10).
12. Pandey M, Kosey S, Garg R. Drug Utilization Review on Corticosteroids Use in a Tertiary Care Teaching Hospital. Int J Sci Res Knowledge 2015;3(12):0305-3.
13. Dhandapani C, Arulkumaran KSG, Asha P. Drug Utilization Evaluation of Corticosteroids Based on Safety: A Prospective Observational Study. IJPTP 2015;6(1):1591-7.
14. Ni YN, Chen G, Sun J et al. The effect of corticosteroids on mortality of patients with influenza pneumonia: a systematic review and meta-analysis. Crit Care 2019;23:99.
15. Peterson RW. Assessing the efficacy and safety of medical technologies. 1978.
16. Vinay BC, Shastry CS, Kodangala S et al. Development and validation of patient information leaflet for coronary heart disease patients. Perspect Clin Res 2021;(12):83-6.
17. Jarad NA, Wedzicha JA, Burge PS. An Observational study of inhaled corticosteroid withdrawal in stable chronic obstructive pulmonary disease. Respir Med 1999;(93):161-6.
18. Parikh A, Scadding GK, Darby Y et al. Topical corticosteroids in chronic rhinosinusitis: a randomized, double-blind, placebo-controlled trial using fluticasone propionate aqueous nasal spray. Rhinology 2001;(39):75-9.
19. Shazma Imam, Priti Sharma, Dinesh Kumar Mehta et al. Corticosteroid Utilization pattern: A Prospective study at a tertiary teaching Hospital. Research. J. pharm. and Tech. 13 (8): August 2020
20. Silver J, Bogart M, Packnett E et al. Real-World Reductions in Oral Corticosteroid Use in the USA Following Mepolizumab Therapy for Severe Asthma. J Asthma Allergy 2020; р.689-99. DOI: 10.2147/JAA. S275944
21. Yawn BP, Li Y, Tian H et al. Inhaled Corticosteroid use in patients with chronic obstructive pulmonary disease and the risk of pneumonia: a retrospective claims data analysis. Int J COPD 2013; р. 295-304. DOI: 10.2147/COPD.S42366
22. Mahmoodan M, Mahesh NM, Ramdurga B. Drug Utilization Evaluation in Chronic Obstructive Pulmonary Disease Patients. Der Pharmacia Lettre 2017;9(6):153-62.
23. Biondi NL, Samiratedu MM, Highsmith E et al. The Impact of Interprofessional Monitoring and Education on the Usage of Systemic Glucocorticoids in Acute Exacerbations of Chronic Obstructive Pulmonary Disease: A Retrospective, Medication Use Review. Cureus 2019;11(11): e6224. DOI: 10.7759/cureus.6224
24. Shende M, Ghutke B, Panekar D, Kachewar A. Assessment of drug utilization pattern of steroids in a district general hospital in Amravati region. Res Results Pharmacology 2019;5(2):57-64.
25. Rafeeq MM, Murad H. Evaluation of drug utilization pattern for patients of bronchial asthma in a government hospital of Saudi Arabia. Niger J Clin Pract 2017;20:1098-105.
26. Yashashri C Shetty, Piyush Vinchukar, Shraddha More et al. Knowledge and Awareness Regarding Corticosteroids and Effectiveness of Novel steroid Educational Module among people visiting General OPD of a Tertiary Care Hospital. Ind J Pharm Practice 2022;15(1).
27. Rollema C, van Roon EM, Schilder AGM et al. Evaluation of instructions in patient information leaflets for the use of intranasal corticosteroid sprays: an observational study. BMJ Open 2019;9:e026710. DOI: 10.1136/ bmjopen-2018-026710
28. Thadanki M, Kumar CH, Tejaswi M et al. Drug utilisation evaluation of corticosteroids in tertiary care teaching hospital. Int J Pharm Sci Res 2019;10(3):1468-76.