Клинический разбор в общей медицине №11 2025
1 College of Nursing, Al-Bayan University, Baghdad, Iraq;
2 Ishtar Medical Institute, Baghdad, Iraq;
3 Al-Hadi University College, Baghdad, Iraq;
4 College of Nursing, University of Basrah, Basrah, Iraq;
5 Ibn Khaldun Private University College, Baghdad, Iraq;
6 Ibn Sina University of Medical and Pharmaceutical Sciences, Baghdad, Iraq;
7 College of Nursing, University of Baghdad, Baghdad, Iraq;
8 Dijlah University College, Baghdad, Iraq;
9 Al-Kut University College, Al-Kut, Iraq;
10 School of Nursing, Qom University of Medical Sciences, Qom, Iran
bahman.agai@gmail.com
Аннотация
Введение. Детям в больницах и детских садах выполняют болезненные процедуры. Существуют разные способы управления болью у детей, в том числе медикаментозные и немедикаментозные, что позволяет сравнить все аспекты лечения боли у детей.
Методы. Выполнен обзор публикаций в базах данных PubMed, Scopus, Web of Science, Science Direct и Google Scholar за 2000–2025 гг. посредством поиска по ключевым словам: «медикаментозные методы лечения», «немедикаментозные методы лечения», «детский» и «инвазивные процедуры». Для первичного анализа из баз данных были извлечены 2400 статей, которые были добавлены в программу по управлению библиографическими списками (EndNote).
Результаты. Критериям включения соответствовали 13 статей. Эти исследования выявили 17 основных проблем. С точки зрения эффективности медикаментозные методы больше подходят для лечения острой боли и тяжелого болевого синдрома, в то время как немедикаментозные методы больше подходят для лечения хронической боли и менее тяжелого болевого синдрома.
Выводы. Полученные результаты позволяют сделать вывод, что медикаментозные и немедикаментозные методы имеют свои преимущества и недостатки. Однако выбор правильного метода зависит от факторов окружающей среды, тяжести боли у ребенка и доступности метода. Учитывая важность управления болью у детей немедикаментозными методами, необходимы стратегии преодоления или уменьшения трудностей. Для решения этих проблем и преодоления трудностей необходимо применять разнообразные подходы в различных областях, включая работу с персоналом, образование, менеджмент и экологию.
Ключевые слова: медикаментозное и немедикаментозное лечение, боль, педиатрический, инвазивные процедуры.
Для цитирования: Азиз А.Р., Худур Х.М., Шухата М.Х., Сауд А.Т., Али М.M.A., Абдулвахид А.С., Аль-Мусаи К. Матшер, Карагул А.Р.М., Хадер Л.К., Кадем Х.М., Убейд Х.А., Кадим А.Д., Бахман А. Медикаментозные и немедикаментозные методы лечения боли у детей после инвазивных процедур: всесторонний сравнительный анализ. Клинический разбор в общей медицине. 2025; 6 (11): 21–26. DOI: 10.47407/kr2025.6.11.00706
Introduction
Pain is a condition characterized by severe discomfort experienced due to an injury or damage to a part of the body. Severe and uncontrollable pain should be considered a medical emergency [1]. Assessing the level of pain experienced by a child plays a crucial role in determining the urgency of treatment [2]. Assessing and recording the level of pain using appropriate scales is necessary not only to determine the presence of pain but also to assess the response to treatment [3]. Children in hospitals and day-care centers often undergo painful procedures [4].
Pain from invasive acts in children is often overlooked, although it may be hidden because of the risk of a subsequent invasive act [5]. Clinical studies show that the lack of pain control in children may lead to long-term effects. In children whose pain is severe enough to require treatment, pain can adversely affect physical and mental health [6]. Fear of pain and injury is one of the most important problems for diseased children, and the fear of painful medical procedures is more common in children than in adults [7]. This fear prevents individuals from receiving appropriate medical care. Children often describe this procedure as the most stressful and one of the most painful aspects of their hospital stay [8]. Children cry, fear, and refuse to cooperate in this condition. Negative responses and psychological distress can cause more problems and lower the success rate in the venipuncture procedure [9]. Pain management in children requires more skill than in adults, who may not be able to verbalize pain without nonverbal cues [10]. This should be tailored to the child's age, developmental stage, maturity, previous pain exposure and experience, and the type and severity of pain currently experienced in childhood [11].
In the past, the common belief was that children did not experience pain and did not feel it properly, which led to many children undergoing surgery without receiving adequate analgesia or sedation [12]. Today, with the advancement of knowledge and the dissemination of various methods, more attention is paid to child pain, which has led to a great deal of progress in pediatric pain control [13].
Many studies have suggested that different Non-pharmacological methods of pain control should be selected according to the child's age. Given the existence of multiple options with appropriate efficiency and the absence of risk in using non-pharmacological methods, one or more suitable distraction methods may be used according to the child's condition [8]. Some non-pharmacological methods, such as distraction, relaxation, skin stimulation, etc., make the patient more comfortable with the pain and make it more bearable. Another benefit of these methods is that they increase the effectiveness of painkillers, which reduces the amount of medication needed [4]. These methods also reduce fear and anxiety, creating a sense of control in the individual, which leads to greater comfort, improved sleep, and rest [14].
Another method is to use pharmacological treatments, in which non-narcotic analgesics are among the therapeutic measures of pain control in children. The use of these drugs provides adequate analgesia for mild to moderate pain and also reduces the need for opioids to control moderate to severe pain [3]. These drugs can be used in different situations, just like non-narcotic methods of pain control. Another category of drug treatment for controlling pain in children is opioids. Opioids play an important role in the treatment of moderate to severe pain and even in controlling pain around surgery and other painful procedures in children [15].
Despite the importance of pain control, research shows that pediatric pain is still not well managed. Research findings are contradictory, each addressing a different aspect of non-pharmacological methods. By analyzing prior studies, it aims to provide a comprehensive comparative all aspects of pediatric pain treatment for two methods, and evaluate them in terms of practical challenges in clinical field.
Instrument and Methods
Study design
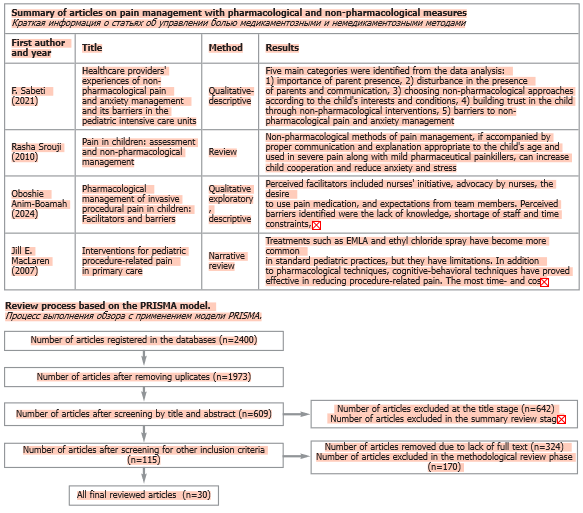
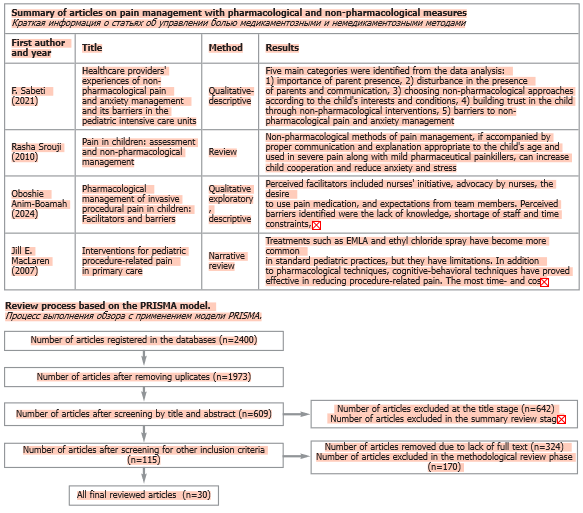
This comprehensive review aimed to compare pharmacological and non-pharmacological treatments in children undergoing invasive procedures. We followed (PRISMA) in Figure, for this purpose, the databases PubMed, Scopus, Web of Science, ScienceDirect, and Google Scholar were searched using the keywords on MeSH "pharmacological treatments of pain", "non-pharmacological treatments of pain", "pediatric" and "invasive procedures" between 2000 and 2025. Studies were reviewed for their titles and abstracts. In the initial review, 2200 articles were retrieved and then added to a reference management software (EndNote). After removing duplicates and irrelevant items based on an evaluation of the title, abstract, and full text, 30 articles were finally included for discussion.
Findings
Study selection
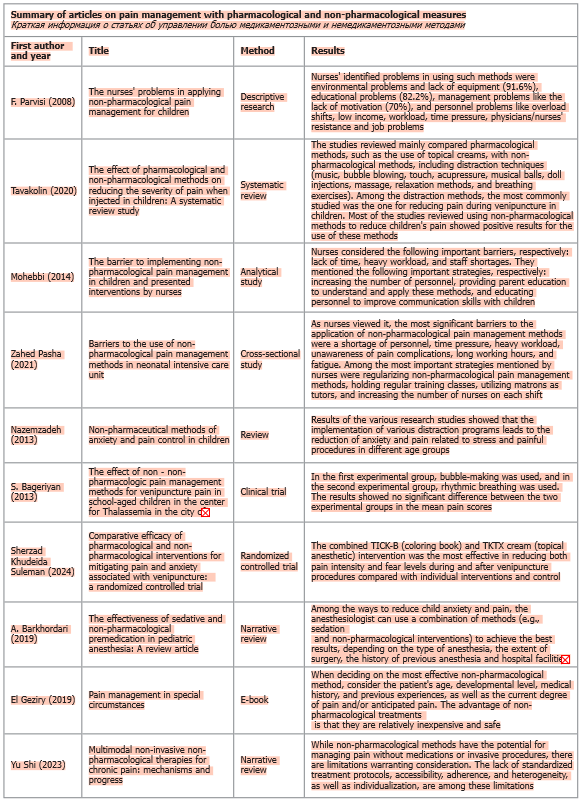
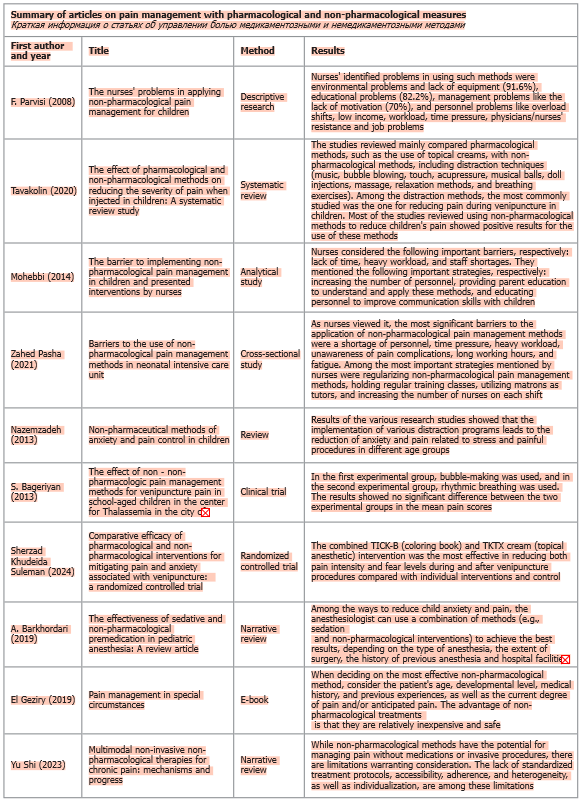
A total number of about 30 articles were reviewed in this study. The results of the review of these articles are presented in two parts. First, the pharmacological and non-pharmacological methods for controlling pain in children are given. Then, in Table, a number of the most important articles reviewed are presented, which compare these two methods of pain control. In the discussion section, other articles are analyzed, and their findings are interpreted.
A. Non-pharmacological treatments
In general, non-pharmacological methods include music therapy, aromatherapy, cold therapy, heat therapy, massage therapy, oxygen therapy, relaxation, touch therapy, water therapy, distraction, yoga, transcutaneous electrical nerve stimulation, and the use of herbal medicine [8]. Non-pharmacological pediatric solutions included robotic technology, watching cartoons, educational videos, the presence of mothers, breastfeeding, the mother's voice, audiovisual tools, music therapy, and pressure techniques. The effect of play therapy on pain control in children has also been proven [13]. In various studies, the role of several methods, such as hypnosis, thought diversion, and guided thoughts and images, in reducing pain has been used or emphasized for children. Among them, thought diversion is the most common method for painless procedures that last for a short time [15]. Thought diversion involves engaging the child in various types of activities, helping them focus their attention on something other than the care procedure. Therefore, the tactics used to reduce pain sensitivity in children include thought diversion and utilizing the five senses [16]. Examples of distraction activities include listening to music, singing, playing games, watching television, blowing bubbles, and 3D imaging. Despite the variety of methods, it is best to choose an activity that is developmentally appropriate for the child. Using distraction methods is as effective as, or even better than, pharmacological methods [17].
B. Pharmacological treatments
There are various drugs for pain relief. Acetaminophen and non-steroidal anti-inflammatory drugs (NSAIDs) are among the most commonly prescribed medications during pediatric hospitalizations to control mild to moderate pain [18]. A variety of opioid medications are available to treat pain in pediatrics and are recommended by WHO in combination with non-opioid analgesics to treat moderate to severe pain resulting from acute and chronic pain syndromes [19]. Narcotic drugs bind to the central nervous system's opioid receptors and block or alter the transmission of pain signals. Drugs such as codeine and morphine are among these drugs [20]. Major sedatives, minor sedatives, and tricyclic antidepressants have all been used as adjuncts in pain management. Benzodiazepines are relatively safe and reduce pain associated with anxiety [21].
Discussions
Although pharmacological and non-pharmacological pain control treatments are comparable in several aspects according to the purpose of this study, the main indicators used in this study include cost and availability, practical challenges, effectiveness, and complications, as discussed separately below, and the results are compared.
Cost and availability
The use of non-pharmacological methods of pain relief is preferable to pharmacological methods in terms of cost and availability. Therefore, it is noteworthy that in cases where pharmacological methods of pain relief are not available, non-pharmacological methods of pain relief can be used [16]. In their study, А. Alavi et al. (2005) compared the effects of thought distortion and artificial insemination on the severity of phlebotomy pain in 5- to 12-year-old children with thalassemia. The results showed that both EMLA cream and distraction reduce the pain of phlebotomy. However, considering that thought distortion is more economical than EMLA cream, the use of this method is recommended [17]. В. Pouraboli et al. (2016) showed that pressure on the Huko point leads to reduced behavioral responses to pain intensity due to catheter insertion in children with Thalassemia, and it is a cheap, easy, and non-invasive method [8].
Practical challenges
Nurses cited issues such as excessive working hours, time and work pressure, staff shortages, inadequate training, lack of ongoing refresher courses, and the absence of mothers during procedures as barriers to using non-pharmacological pain control methods [18–21].
In their study, F. Parvizi et al. (2008) investigated the level of nurses' knowledge regarding non-pharmacological methods for managing child pain. The results showed that 99% of nurses had not received any training on the non-pharmacological methods of pain control in children during training. Moreover, 82.6% cited the lack of refresher courses as one reason for not using these methods [22]. In another study, P. Byrd et al. (2009) showed that barriers to non-pharmacological pain management include the lack of pain management protocols, nurse and physician resistance, and inadequate training for staff in assessing and managing pain. The researchers concluded that a gap exists in knowledge and practice regarding pain management and that increased education for caregivers is necessary [23]. Routinizing non-pharmacological methods of pain control, holding continuing education classes, increasing the number of nurses per shift or reducing nurse working hours, providing the right equipment for implementing this method, providing pain control sheets, encouraging successful nurses, forming pain management committees in hospitals, adding the topic of pain control management to nursing courses, and reducing resistance from doctors and nurses are strategies to increase use and reduce barriers to non-pharmacological methods [24, 25].
Effectiveness
The use of non-pharmacological treatments increases the patient's coping ability, reduces anxiety, and can be used easily by children. W. Zempsky et al. (2008) compared two methods of music and EMLA anesthetic cream in controlling the intensity of pain caused by venipuncture in children [26]. M. Shahabi et al. (2006) compared the effect of anesthetic ointment on pain caused by local anesthetic and distraction of thought (music) during venipuncture in school-age children. They reported that the use of ointment on pain during venipuncture in school-age children was significantly associated with the use of music and distraction of thought (music), and each of these methods could replace the other [27]. However, M. Hazinski et al. (2012) showed when a child had very severe pain, distraction might not be very effective [28]. M. Namnabati et al. (2002) demonstrated that various distractions can cause individuals to redirect or change the focus of their method. Generally, distraction is one way to focus one's attention on a stimulus, and these external processes in the environment are directed toward a stimulus other than pain, which relieves the feeling of pain [29]. In contrast, if one is provided with diverse activities, such as watching cartoons, one's attention is attracted to them and is prevented from dealing with the pain, resulting in a feeling of less pain [2]. In other words, increasing other sensory stimuli, primarily auditory, visual, tactile, and positional, can lead to a change in response. Distraction refers to one's attention away from pain and one's sensory and emotional reactions to a painful stimulus [13].
Side effects and complications
Pain relief with non-pharmacological methods is not only cost-effective but also non-invasive and depends solely on the nurse's performance [3]. Side effects of painkillers vary as a function of the specific medication used and can include nausea/vomiting, constipation, itching, irritation (especially in young children), and many more [30]. Non-pharmacological treatments allow the child to play an active role during treatment, to overcome the feeling of victimization, and to have a sense of authority and control over responses to the situation [20]. These methods also reduce fear and anxiety, creating a sense of control in the individual, which in turn fosters greater comfort and improves sleep and rest. As M. Shaban et al. (2006) found and reported, non-pharmacological treatments reduce the use of painkillers and narcotics, which can have side effects such as respiratory problems, respiratory distress, cough, and even addiction and dependence [31].
Conclusion
As the present findings show, although both pharmacological and non-pharmacological methods have advantages and disadvantages, selecting the proper method depends on environmental factors, the child's pain status, and access to that method. Pharmacological treatments better suit severe pain and emergencies, and non-pharmacological treatments are better for non-emergency conditions as they also reduce the child's anxiety level and do not eliminate pain but rather reduce its perception. Considering the importance of non-pharmacological pain control in children without causing any side effects and creating a sense of calm and comfort, there is a need for strategies to reduce or eliminate barriers to using them. Addressing these problems and barriers requires multiple approaches in various areas, including personnel, education, management, and the environment.
Ethics approval. Given that our research is a review study and no animal or human intervention was performed in this study, no code of ethics was received from the Ethics Committee of the University of Baghdad.
Funding. No funding was received for this study.
Availability of data and materials. The data utilized to support the results of the research are accessible to the corresponding author upon request.
Conflicts of interest. The authors declare no conflict of interest.
Competing interests. The authors declare no competing interests.
Одобрение этического комитета. С учетом того, что работа представляет собой обзор, который не предполагает использование животных или участие людей, одобрение этического комитета Багдадского университета не требуется.
Финансирование. Исследование выполнено без финансовой поддержки.
Доступность данных и материалов. Данные, использованные для подтверждения результатов исследования, доступны по запросу на имя ответственного автора.
Конфликт интересов. Авторы заявляют об отсутствии конфликта интересов.
Конкурирующие интересы. Авторы заявляют об отсутствии конкурирующих интересов.
Information about the authors
Информация об авторах
Afifa Radha Aziz – PhD Nursing, Professor, Department of Paediatric Nursing, College of Nursing, Al-Bayan University. E-mail: afifa.r@albayan.edu.iq; ORCID: 0009-0002-6069-692X
Афифа Радха Азиз – PhD по сестринскому делу, проф. каф. сестринского дела в педиатрии, Колледж медицинских сестер, Университет Аль-Баян. E-mail: afifa.r@albayan.edu.iq; ORCID: 0009-0002-6069-692X
Khalida Mohammed Khudur – PhD Nursing, Professor, Ishtar Medical Institute. E-mail: Khalida.Mohammed@ishtar.edu.iq;
ORCID: 0000-0002-3490-0264
Халида Мохаммед Худур – PhD по сестринскому делу, проф. Медицинского института Иштар. E-mail: Khalida.Mohammed@ishtar.edu.iq; ORCID: 0000-0002-3490-0264
Mahmood Hasen Shuhata – Al-Hadi University College. E-mail: Dp.dentistryb@huc.edu.iq
Махмуд Хасен Шухата – Университетский колледж Аль-Хади. E-mail: Dp.dentistryb@huc.edu.iq
Ahmed T. Saud – PhD, Department Fundamentals of Nursing, College of Nursing, University of Basrah. E-mail: Ahmed.saud@uobasrah.edu.iq; ORCID: 0000-0002-0292-0746
Ахмед Т. Сауд – PhD, каф. основ сестринского дела, Колледж медицинских сестер, Университет Басры. E-mail: Ahmed.saud@uobasrah.edu.iq; ORCID: 0000-0002-0292-0746
Majeed M.A. Ali – PhD, Ibn Khaldun Private University College.
E-mail: Dr.majeed@ik.edu.iq
Маджид M.A. Али – PhD, Частный университетский колледж Халдун. E-mail: Dr.majeed@ik.edu.iq
Alzahraa S. Abdulwahid – MSc, Ibn Sina University of Medical and Pharmaceutical Science. E-mail: alzahraa.sabah@ibnsina.edu.iq; ORCID: 0000-0001-9238-9428
Альзахра С. Абдулвахид – магистр, Университет медицинских и фармацевтических наук имени Ибн Сина. E-mail: alzahraa.sabah@ibnsina.edu.iq; ORCID: 0000-0001-9238-9428
Al-Musawi K. Matsher – Professor, Pediatric Health Nursing, College of Nursing, University of Baghdad.
E-mail: dr.khatam@conursing.uobaghdad.edu.iq
Аль-Мусаи К. Матшер – профессор, Колледж медицинских сестер, Багдадский университет. E-mail: dr.khatam@conursing.uobaghdad.edu.iq
Anas Ramaid Mohammad Karaghool – MSc, Community Health Nursing, Radiology Techniques Department, Dijlah University College. E-mail: anas.ramaid@duc.edu.iq; ORCID: 0009-0006-0670-043X
Анас Рамаид Мохаммед Карагул – магистр, сестринское дело в общественном здравоохранении, каф. радиологии, Университетский колледж Диджла. E-mail: anas.ramaid@duc.edu.iq; ORCID: 0009-0006-0670-043X
Lubna Qassim Khader – MSc, Pediatric Nursing, Anesthesia Techniques Department, Dijlah University College. E-mail: lubna.qassim@duc.edu.iq; ORCID: 0009-0005-8089-1820
Лубна Касем Хадер – магистр, сестринское дело в общественном здравоохранении, каф. радиологии, Университетский колледж Диджла. E-mail: E-mail: lubna.qassim@duc.edu.iq; ORCID: 0009-0005-8089-1820
Haider Mansour Kadhem – MSc, Nursing, Assistant Lecturer, Department of Nursing, Al-Kut University College. E-mail: Haider.daham@alkutcollege.edu.iq; ORCID: 0009-0007-8717-241X
Хейдер Мансур Кадем – магистр, сестринское дело, ассистент каф. сестринского дела, Университетский колледж Аль-Кут. E-mail: Haider.daham@alkutcollege.edu.iq; ORCID: 0009-0007-8717-241X
Hussein Aadi Ubaid – PhD Nursing, Lecturer, Department of Adult Nursing, Al-Kut University College. E-mail: Hussein.Ubaid@alkutcollege.edu.iq; ORCID: 0009-0003-9299-4179
Хуссейн Аади Убейд – PhD по сестринскому делу, преподаватель каф. сестринского ухода за взрослыми пациентами, Университетский колледж Аль-Кут. E-mail: Hussein.Ubaid@alkutcollege.edu.iq; ORCID: 0009-0003-9299-4179
Alaa Jawad Kadhim – PhD Nursing, Assistant Professor, Department of Adult Nursing, College of Nursing, University of Baghdad. E-mail: alaaj@conursing.uobaghdad.edu.iq; ORCID: 0000-0002-4306-6830
Алаа Джавад Кадим – PhD по сестринскому делу, доц. каф. сестринского ухода за взрослыми пациентами, Багдадский университет. E-mail: alaaj@conursing.uobaghdad.edu.iq; ORCID: 0000-0002-4306-6830
Aghaie Bahman – PhD, Associate Professor, Department of Medical-Surgical Nursing, School of Nursing, Qom University of Medical Sciences. E-mail: bahman.agai@gmail.com; ORCID: 0000-0002-2267-2700
Агхеие Бахман – PhD, доц. каф. сестринского дела в хирургии, Школа медицинских сестер, Университет медицинских наук Кум. E-mail: bahman.agai@gmail.com; ORCID: 0000-0002-2267-2700
Received: 31.10.2025
Revised: 05.11.2025
Accepted: 06.11.2025
Поступила в редакцию: 31.10.2025
Поступила после рецензирования: 05.11.2025
Принята к публикации: 06.11.2025
Клинический разбор в общей медицине №11 2025
Медикаментозные и немедикаментозные методы лечения боли у детей после инвазивных процедур: всесторонний сравнительный анализ
Номера страниц в выпуске:21-26
Abstract
Background. Children in hospitals and day-care centers undergo painful procedures. There are different ways of controlling pain in children, including pharmacological and non-pharmacological treatments, to compare all aspects of pediatric pain treatment.
Methods. A review was conducted across databases PubMed, Scopus, Web of Science, Science Direct, and Google Scholar were searched using the keywords "pharmacological treatments", "non-pharmacological treatments", "pediatric" and "invasive procedures" between 2000 and 2025. In the initial review, 2400 articles were retrieved and then added to a reference management software (EndNote).
Results. Thirteen articles met the inclusion criteria these studies highlighted seventeen key challenges. In terms of effectiveness, the pharmacological method has more support for acute and severe pain, while the non-pharmacological method enjoys more support for chronic and less severe pain.
Conclusion. The findings, it can be concluded that both pharmacological and non-pharmacological methods have advantages and disadvantages. Yet, selecting the proper method depends on environmental factors, the child's pain status, and access to that method. Considering the importance of non-pharmacological pain control in children, there is a need for strategies to remove or reduce obstacles. Addressing these problems and obstacles requires multiple approaches in various areas, including personnel, education, management, and the environment.
Keywords: pharmacological and non-pharmacological treatments, pain, pediatric, invasive procedures.
For citation: Aziz A.R., Khudur Kh.M., Shuhata M.H., Saud A.T., Ali M.M.A., Abdulwahid A.S., Al-Musawi K. Matsher, Karaghool A.R.M., Khader L.Q., Kadhem H.M., Ubaid H.A., Kadhim A.J., Bahman A. Pharmacological and non-pharmacological treatments for pain management in children undergoing invasive procedures: a comprehensive comparative review. Clinical review for general practice. 2025; 6 (11): 21–26. DOI: 10.47407/kr2025.6.11.00706
Background. Children in hospitals and day-care centers undergo painful procedures. There are different ways of controlling pain in children, including pharmacological and non-pharmacological treatments, to compare all aspects of pediatric pain treatment.
Methods. A review was conducted across databases PubMed, Scopus, Web of Science, Science Direct, and Google Scholar were searched using the keywords "pharmacological treatments", "non-pharmacological treatments", "pediatric" and "invasive procedures" between 2000 and 2025. In the initial review, 2400 articles were retrieved and then added to a reference management software (EndNote).
Results. Thirteen articles met the inclusion criteria these studies highlighted seventeen key challenges. In terms of effectiveness, the pharmacological method has more support for acute and severe pain, while the non-pharmacological method enjoys more support for chronic and less severe pain.
Conclusion. The findings, it can be concluded that both pharmacological and non-pharmacological methods have advantages and disadvantages. Yet, selecting the proper method depends on environmental factors, the child's pain status, and access to that method. Considering the importance of non-pharmacological pain control in children, there is a need for strategies to remove or reduce obstacles. Addressing these problems and obstacles requires multiple approaches in various areas, including personnel, education, management, and the environment.
Keywords: pharmacological and non-pharmacological treatments, pain, pediatric, invasive procedures.
For citation: Aziz A.R., Khudur Kh.M., Shuhata M.H., Saud A.T., Ali M.M.A., Abdulwahid A.S., Al-Musawi K. Matsher, Karaghool A.R.M., Khader L.Q., Kadhem H.M., Ubaid H.A., Kadhim A.J., Bahman A. Pharmacological and non-pharmacological treatments for pain management in children undergoing invasive procedures: a comprehensive comparative review. Clinical review for general practice. 2025; 6 (11): 21–26. DOI: 10.47407/kr2025.6.11.00706
Медикаментозные и немедикаментозные методы лечения боли у детей после инвазивных процедур: всесторонний сравнительный анализ
Afifa Radha Aziz1, Khalida Mohammed Khudur2, Mahmood Hasen Shuhata3, Ahmed T. Saud4, Majeed M.A. Ali5, Alzahraa S. Abdulwahid6, Khatam M. Hattab7, Anas Ramaid Mohammad Karaghool8, Lubna Qassim Khader8, Haider Mansour Kadhem9, Hussein Aadi Ubaid9, Alaa Jawad Kadhim7, Aghaie Bahman101 College of Nursing, Al-Bayan University, Baghdad, Iraq;
2 Ishtar Medical Institute, Baghdad, Iraq;
3 Al-Hadi University College, Baghdad, Iraq;
4 College of Nursing, University of Basrah, Basrah, Iraq;
5 Ibn Khaldun Private University College, Baghdad, Iraq;
6 Ibn Sina University of Medical and Pharmaceutical Sciences, Baghdad, Iraq;
7 College of Nursing, University of Baghdad, Baghdad, Iraq;
8 Dijlah University College, Baghdad, Iraq;
9 Al-Kut University College, Al-Kut, Iraq;
10 School of Nursing, Qom University of Medical Sciences, Qom, Iran
bahman.agai@gmail.com
Аннотация
Введение. Детям в больницах и детских садах выполняют болезненные процедуры. Существуют разные способы управления болью у детей, в том числе медикаментозные и немедикаментозные, что позволяет сравнить все аспекты лечения боли у детей.
Методы. Выполнен обзор публикаций в базах данных PubMed, Scopus, Web of Science, Science Direct и Google Scholar за 2000–2025 гг. посредством поиска по ключевым словам: «медикаментозные методы лечения», «немедикаментозные методы лечения», «детский» и «инвазивные процедуры». Для первичного анализа из баз данных были извлечены 2400 статей, которые были добавлены в программу по управлению библиографическими списками (EndNote).
Результаты. Критериям включения соответствовали 13 статей. Эти исследования выявили 17 основных проблем. С точки зрения эффективности медикаментозные методы больше подходят для лечения острой боли и тяжелого болевого синдрома, в то время как немедикаментозные методы больше подходят для лечения хронической боли и менее тяжелого болевого синдрома.
Выводы. Полученные результаты позволяют сделать вывод, что медикаментозные и немедикаментозные методы имеют свои преимущества и недостатки. Однако выбор правильного метода зависит от факторов окружающей среды, тяжести боли у ребенка и доступности метода. Учитывая важность управления болью у детей немедикаментозными методами, необходимы стратегии преодоления или уменьшения трудностей. Для решения этих проблем и преодоления трудностей необходимо применять разнообразные подходы в различных областях, включая работу с персоналом, образование, менеджмент и экологию.
Ключевые слова: медикаментозное и немедикаментозное лечение, боль, педиатрический, инвазивные процедуры.
Для цитирования: Азиз А.Р., Худур Х.М., Шухата М.Х., Сауд А.Т., Али М.M.A., Абдулвахид А.С., Аль-Мусаи К. Матшер, Карагул А.Р.М., Хадер Л.К., Кадем Х.М., Убейд Х.А., Кадим А.Д., Бахман А. Медикаментозные и немедикаментозные методы лечения боли у детей после инвазивных процедур: всесторонний сравнительный анализ. Клинический разбор в общей медицине. 2025; 6 (11): 21–26. DOI: 10.47407/kr2025.6.11.00706
Introduction
Pain is a condition characterized by severe discomfort experienced due to an injury or damage to a part of the body. Severe and uncontrollable pain should be considered a medical emergency [1]. Assessing the level of pain experienced by a child plays a crucial role in determining the urgency of treatment [2]. Assessing and recording the level of pain using appropriate scales is necessary not only to determine the presence of pain but also to assess the response to treatment [3]. Children in hospitals and day-care centers often undergo painful procedures [4].
Pain from invasive acts in children is often overlooked, although it may be hidden because of the risk of a subsequent invasive act [5]. Clinical studies show that the lack of pain control in children may lead to long-term effects. In children whose pain is severe enough to require treatment, pain can adversely affect physical and mental health [6]. Fear of pain and injury is one of the most important problems for diseased children, and the fear of painful medical procedures is more common in children than in adults [7]. This fear prevents individuals from receiving appropriate medical care. Children often describe this procedure as the most stressful and one of the most painful aspects of their hospital stay [8]. Children cry, fear, and refuse to cooperate in this condition. Negative responses and psychological distress can cause more problems and lower the success rate in the venipuncture procedure [9]. Pain management in children requires more skill than in adults, who may not be able to verbalize pain without nonverbal cues [10]. This should be tailored to the child's age, developmental stage, maturity, previous pain exposure and experience, and the type and severity of pain currently experienced in childhood [11].
In the past, the common belief was that children did not experience pain and did not feel it properly, which led to many children undergoing surgery without receiving adequate analgesia or sedation [12]. Today, with the advancement of knowledge and the dissemination of various methods, more attention is paid to child pain, which has led to a great deal of progress in pediatric pain control [13].
Many studies have suggested that different Non-pharmacological methods of pain control should be selected according to the child's age. Given the existence of multiple options with appropriate efficiency and the absence of risk in using non-pharmacological methods, one or more suitable distraction methods may be used according to the child's condition [8]. Some non-pharmacological methods, such as distraction, relaxation, skin stimulation, etc., make the patient more comfortable with the pain and make it more bearable. Another benefit of these methods is that they increase the effectiveness of painkillers, which reduces the amount of medication needed [4]. These methods also reduce fear and anxiety, creating a sense of control in the individual, which leads to greater comfort, improved sleep, and rest [14].
Another method is to use pharmacological treatments, in which non-narcotic analgesics are among the therapeutic measures of pain control in children. The use of these drugs provides adequate analgesia for mild to moderate pain and also reduces the need for opioids to control moderate to severe pain [3]. These drugs can be used in different situations, just like non-narcotic methods of pain control. Another category of drug treatment for controlling pain in children is opioids. Opioids play an important role in the treatment of moderate to severe pain and even in controlling pain around surgery and other painful procedures in children [15].
Despite the importance of pain control, research shows that pediatric pain is still not well managed. Research findings are contradictory, each addressing a different aspect of non-pharmacological methods. By analyzing prior studies, it aims to provide a comprehensive comparative all aspects of pediatric pain treatment for two methods, and evaluate them in terms of practical challenges in clinical field.
Instrument and Methods
Study design
This comprehensive review aimed to compare pharmacological and non-pharmacological treatments in children undergoing invasive procedures. We followed (PRISMA) in Figure, for this purpose, the databases PubMed, Scopus, Web of Science, ScienceDirect, and Google Scholar were searched using the keywords on MeSH "pharmacological treatments of pain", "non-pharmacological treatments of pain", "pediatric" and "invasive procedures" between 2000 and 2025. Studies were reviewed for their titles and abstracts. In the initial review, 2200 articles were retrieved and then added to a reference management software (EndNote). After removing duplicates and irrelevant items based on an evaluation of the title, abstract, and full text, 30 articles were finally included for discussion.
Findings
Study selection
A total number of about 30 articles were reviewed in this study. The results of the review of these articles are presented in two parts. First, the pharmacological and non-pharmacological methods for controlling pain in children are given. Then, in Table, a number of the most important articles reviewed are presented, which compare these two methods of pain control. In the discussion section, other articles are analyzed, and their findings are interpreted.
A. Non-pharmacological treatments
In general, non-pharmacological methods include music therapy, aromatherapy, cold therapy, heat therapy, massage therapy, oxygen therapy, relaxation, touch therapy, water therapy, distraction, yoga, transcutaneous electrical nerve stimulation, and the use of herbal medicine [8]. Non-pharmacological pediatric solutions included robotic technology, watching cartoons, educational videos, the presence of mothers, breastfeeding, the mother's voice, audiovisual tools, music therapy, and pressure techniques. The effect of play therapy on pain control in children has also been proven [13]. In various studies, the role of several methods, such as hypnosis, thought diversion, and guided thoughts and images, in reducing pain has been used or emphasized for children. Among them, thought diversion is the most common method for painless procedures that last for a short time [15]. Thought diversion involves engaging the child in various types of activities, helping them focus their attention on something other than the care procedure. Therefore, the tactics used to reduce pain sensitivity in children include thought diversion and utilizing the five senses [16]. Examples of distraction activities include listening to music, singing, playing games, watching television, blowing bubbles, and 3D imaging. Despite the variety of methods, it is best to choose an activity that is developmentally appropriate for the child. Using distraction methods is as effective as, or even better than, pharmacological methods [17].
B. Pharmacological treatments
There are various drugs for pain relief. Acetaminophen and non-steroidal anti-inflammatory drugs (NSAIDs) are among the most commonly prescribed medications during pediatric hospitalizations to control mild to moderate pain [18]. A variety of opioid medications are available to treat pain in pediatrics and are recommended by WHO in combination with non-opioid analgesics to treat moderate to severe pain resulting from acute and chronic pain syndromes [19]. Narcotic drugs bind to the central nervous system's opioid receptors and block or alter the transmission of pain signals. Drugs such as codeine and morphine are among these drugs [20]. Major sedatives, minor sedatives, and tricyclic antidepressants have all been used as adjuncts in pain management. Benzodiazepines are relatively safe and reduce pain associated with anxiety [21].
Discussions
Although pharmacological and non-pharmacological pain control treatments are comparable in several aspects according to the purpose of this study, the main indicators used in this study include cost and availability, practical challenges, effectiveness, and complications, as discussed separately below, and the results are compared.
Cost and availability
The use of non-pharmacological methods of pain relief is preferable to pharmacological methods in terms of cost and availability. Therefore, it is noteworthy that in cases where pharmacological methods of pain relief are not available, non-pharmacological methods of pain relief can be used [16]. In their study, А. Alavi et al. (2005) compared the effects of thought distortion and artificial insemination on the severity of phlebotomy pain in 5- to 12-year-old children with thalassemia. The results showed that both EMLA cream and distraction reduce the pain of phlebotomy. However, considering that thought distortion is more economical than EMLA cream, the use of this method is recommended [17]. В. Pouraboli et al. (2016) showed that pressure on the Huko point leads to reduced behavioral responses to pain intensity due to catheter insertion in children with Thalassemia, and it is a cheap, easy, and non-invasive method [8].
Practical challenges
Nurses cited issues such as excessive working hours, time and work pressure, staff shortages, inadequate training, lack of ongoing refresher courses, and the absence of mothers during procedures as barriers to using non-pharmacological pain control methods [18–21].
In their study, F. Parvizi et al. (2008) investigated the level of nurses' knowledge regarding non-pharmacological methods for managing child pain. The results showed that 99% of nurses had not received any training on the non-pharmacological methods of pain control in children during training. Moreover, 82.6% cited the lack of refresher courses as one reason for not using these methods [22]. In another study, P. Byrd et al. (2009) showed that barriers to non-pharmacological pain management include the lack of pain management protocols, nurse and physician resistance, and inadequate training for staff in assessing and managing pain. The researchers concluded that a gap exists in knowledge and practice regarding pain management and that increased education for caregivers is necessary [23]. Routinizing non-pharmacological methods of pain control, holding continuing education classes, increasing the number of nurses per shift or reducing nurse working hours, providing the right equipment for implementing this method, providing pain control sheets, encouraging successful nurses, forming pain management committees in hospitals, adding the topic of pain control management to nursing courses, and reducing resistance from doctors and nurses are strategies to increase use and reduce barriers to non-pharmacological methods [24, 25].
Effectiveness
The use of non-pharmacological treatments increases the patient's coping ability, reduces anxiety, and can be used easily by children. W. Zempsky et al. (2008) compared two methods of music and EMLA anesthetic cream in controlling the intensity of pain caused by venipuncture in children [26]. M. Shahabi et al. (2006) compared the effect of anesthetic ointment on pain caused by local anesthetic and distraction of thought (music) during venipuncture in school-age children. They reported that the use of ointment on pain during venipuncture in school-age children was significantly associated with the use of music and distraction of thought (music), and each of these methods could replace the other [27]. However, M. Hazinski et al. (2012) showed when a child had very severe pain, distraction might not be very effective [28]. M. Namnabati et al. (2002) demonstrated that various distractions can cause individuals to redirect or change the focus of their method. Generally, distraction is one way to focus one's attention on a stimulus, and these external processes in the environment are directed toward a stimulus other than pain, which relieves the feeling of pain [29]. In contrast, if one is provided with diverse activities, such as watching cartoons, one's attention is attracted to them and is prevented from dealing with the pain, resulting in a feeling of less pain [2]. In other words, increasing other sensory stimuli, primarily auditory, visual, tactile, and positional, can lead to a change in response. Distraction refers to one's attention away from pain and one's sensory and emotional reactions to a painful stimulus [13].
Side effects and complications
Pain relief with non-pharmacological methods is not only cost-effective but also non-invasive and depends solely on the nurse's performance [3]. Side effects of painkillers vary as a function of the specific medication used and can include nausea/vomiting, constipation, itching, irritation (especially in young children), and many more [30]. Non-pharmacological treatments allow the child to play an active role during treatment, to overcome the feeling of victimization, and to have a sense of authority and control over responses to the situation [20]. These methods also reduce fear and anxiety, creating a sense of control in the individual, which in turn fosters greater comfort and improves sleep and rest. As M. Shaban et al. (2006) found and reported, non-pharmacological treatments reduce the use of painkillers and narcotics, which can have side effects such as respiratory problems, respiratory distress, cough, and even addiction and dependence [31].
Conclusion
As the present findings show, although both pharmacological and non-pharmacological methods have advantages and disadvantages, selecting the proper method depends on environmental factors, the child's pain status, and access to that method. Pharmacological treatments better suit severe pain and emergencies, and non-pharmacological treatments are better for non-emergency conditions as they also reduce the child's anxiety level and do not eliminate pain but rather reduce its perception. Considering the importance of non-pharmacological pain control in children without causing any side effects and creating a sense of calm and comfort, there is a need for strategies to reduce or eliminate barriers to using them. Addressing these problems and barriers requires multiple approaches in various areas, including personnel, education, management, and the environment.
Ethics approval. Given that our research is a review study and no animal or human intervention was performed in this study, no code of ethics was received from the Ethics Committee of the University of Baghdad.
Funding. No funding was received for this study.
Availability of data and materials. The data utilized to support the results of the research are accessible to the corresponding author upon request.
Conflicts of interest. The authors declare no conflict of interest.
Competing interests. The authors declare no competing interests.
Одобрение этического комитета. С учетом того, что работа представляет собой обзор, который не предполагает использование животных или участие людей, одобрение этического комитета Багдадского университета не требуется.
Финансирование. Исследование выполнено без финансовой поддержки.
Доступность данных и материалов. Данные, использованные для подтверждения результатов исследования, доступны по запросу на имя ответственного автора.
Конфликт интересов. Авторы заявляют об отсутствии конфликта интересов.
Конкурирующие интересы. Авторы заявляют об отсутствии конкурирующих интересов.
Information about the authors
Информация об авторах
Afifa Radha Aziz – PhD Nursing, Professor, Department of Paediatric Nursing, College of Nursing, Al-Bayan University. E-mail: afifa.r@albayan.edu.iq; ORCID: 0009-0002-6069-692X
Афифа Радха Азиз – PhD по сестринскому делу, проф. каф. сестринского дела в педиатрии, Колледж медицинских сестер, Университет Аль-Баян. E-mail: afifa.r@albayan.edu.iq; ORCID: 0009-0002-6069-692X
Khalida Mohammed Khudur – PhD Nursing, Professor, Ishtar Medical Institute. E-mail: Khalida.Mohammed@ishtar.edu.iq;
ORCID: 0000-0002-3490-0264
Халида Мохаммед Худур – PhD по сестринскому делу, проф. Медицинского института Иштар. E-mail: Khalida.Mohammed@ishtar.edu.iq; ORCID: 0000-0002-3490-0264
Mahmood Hasen Shuhata – Al-Hadi University College. E-mail: Dp.dentistryb@huc.edu.iq
Махмуд Хасен Шухата – Университетский колледж Аль-Хади. E-mail: Dp.dentistryb@huc.edu.iq
Ahmed T. Saud – PhD, Department Fundamentals of Nursing, College of Nursing, University of Basrah. E-mail: Ahmed.saud@uobasrah.edu.iq; ORCID: 0000-0002-0292-0746
Ахмед Т. Сауд – PhD, каф. основ сестринского дела, Колледж медицинских сестер, Университет Басры. E-mail: Ahmed.saud@uobasrah.edu.iq; ORCID: 0000-0002-0292-0746
Majeed M.A. Ali – PhD, Ibn Khaldun Private University College.
E-mail: Dr.majeed@ik.edu.iq
Маджид M.A. Али – PhD, Частный университетский колледж Халдун. E-mail: Dr.majeed@ik.edu.iq
Alzahraa S. Abdulwahid – MSc, Ibn Sina University of Medical and Pharmaceutical Science. E-mail: alzahraa.sabah@ibnsina.edu.iq; ORCID: 0000-0001-9238-9428
Альзахра С. Абдулвахид – магистр, Университет медицинских и фармацевтических наук имени Ибн Сина. E-mail: alzahraa.sabah@ibnsina.edu.iq; ORCID: 0000-0001-9238-9428
Al-Musawi K. Matsher – Professor, Pediatric Health Nursing, College of Nursing, University of Baghdad.
E-mail: dr.khatam@conursing.uobaghdad.edu.iq
Аль-Мусаи К. Матшер – профессор, Колледж медицинских сестер, Багдадский университет. E-mail: dr.khatam@conursing.uobaghdad.edu.iq
Anas Ramaid Mohammad Karaghool – MSc, Community Health Nursing, Radiology Techniques Department, Dijlah University College. E-mail: anas.ramaid@duc.edu.iq; ORCID: 0009-0006-0670-043X
Анас Рамаид Мохаммед Карагул – магистр, сестринское дело в общественном здравоохранении, каф. радиологии, Университетский колледж Диджла. E-mail: anas.ramaid@duc.edu.iq; ORCID: 0009-0006-0670-043X
Lubna Qassim Khader – MSc, Pediatric Nursing, Anesthesia Techniques Department, Dijlah University College. E-mail: lubna.qassim@duc.edu.iq; ORCID: 0009-0005-8089-1820
Лубна Касем Хадер – магистр, сестринское дело в общественном здравоохранении, каф. радиологии, Университетский колледж Диджла. E-mail: E-mail: lubna.qassim@duc.edu.iq; ORCID: 0009-0005-8089-1820
Haider Mansour Kadhem – MSc, Nursing, Assistant Lecturer, Department of Nursing, Al-Kut University College. E-mail: Haider.daham@alkutcollege.edu.iq; ORCID: 0009-0007-8717-241X
Хейдер Мансур Кадем – магистр, сестринское дело, ассистент каф. сестринского дела, Университетский колледж Аль-Кут. E-mail: Haider.daham@alkutcollege.edu.iq; ORCID: 0009-0007-8717-241X
Hussein Aadi Ubaid – PhD Nursing, Lecturer, Department of Adult Nursing, Al-Kut University College. E-mail: Hussein.Ubaid@alkutcollege.edu.iq; ORCID: 0009-0003-9299-4179
Хуссейн Аади Убейд – PhD по сестринскому делу, преподаватель каф. сестринского ухода за взрослыми пациентами, Университетский колледж Аль-Кут. E-mail: Hussein.Ubaid@alkutcollege.edu.iq; ORCID: 0009-0003-9299-4179
Alaa Jawad Kadhim – PhD Nursing, Assistant Professor, Department of Adult Nursing, College of Nursing, University of Baghdad. E-mail: alaaj@conursing.uobaghdad.edu.iq; ORCID: 0000-0002-4306-6830
Алаа Джавад Кадим – PhD по сестринскому делу, доц. каф. сестринского ухода за взрослыми пациентами, Багдадский университет. E-mail: alaaj@conursing.uobaghdad.edu.iq; ORCID: 0000-0002-4306-6830
Aghaie Bahman – PhD, Associate Professor, Department of Medical-Surgical Nursing, School of Nursing, Qom University of Medical Sciences. E-mail: bahman.agai@gmail.com; ORCID: 0000-0002-2267-2700
Агхеие Бахман – PhD, доц. каф. сестринского дела в хирургии, Школа медицинских сестер, Университет медицинских наук Кум. E-mail: bahman.agai@gmail.com; ORCID: 0000-0002-2267-2700
Received: 31.10.2025
Revised: 05.11.2025
Accepted: 06.11.2025
Поступила в редакцию: 31.10.2025
Поступила после рецензирования: 05.11.2025
Принята к публикации: 06.11.2025
Список исп. литературыСкрыть список1. Kotova OV, Borodulina IV. Pain in children and adolescents. Clinical review for general practice 2024;5 (8):79-83. (In Russ.). DOI: 10.47407/kr2024.5.8.00463
2. Dalvandi A, Ranjbar H, Hatamizadeh M et al. Comparing the effectiveness of vapocoolant spray and lidocaine/procaine cream in reducing pain of intravenous cannulation: A randomized clinical trial. Am J Emerg Med 2017;35(8):1064-8.
3. Costello M, Ramundo M, Christopher NC, Powell KR. Ethyl vinyl chloride vapocoolant spray fails to decrease pain associated with intravenous cannulation in children. Clin Pediatr (Phila) 2006;45(7):628-32.
4. Hogan ME, Smart S, Shah V, Taddio A. A systematic review of vapocoolants for reducing pain from venipuncture and venous cannulation in children and adults. J Emerg Med 2014;47(6):736-49.
5. Thrane SE, Wanless S, Cohen SM, Danford CA. The Assessment and Non-Pharmacologic Treatment of Procedural Pain From Infancy to School Age Through a Developmental Lens: A Synthesis of Evidence With Recommendations. J Pediatr Nurs 2016;31(1):e23-32.
6. Groenewald CB, Essner BS, Wright D et al. The economic costs of chronic pain among a cohort of treatment-seeking adolescents in the United States. J Pain 2014;15(9):925-33.
7. Harrington JW, Logan S, Harwell C et al. Effective analgesia using physical interventions for infant immunizations. Pediatrics 2012;129(5):815-22.
8. Pouraboli B, Abazari F, Rostami M, Jahani Y. Effect of pressure of Huko point on behavioural responses to pain during Catheter insertion in children with thalassemia. Iran J Pediatr Nurs 2016;2(3):17-24.
9. Von Baeyer CL, Forsyth SJ, Stanford EA et al. Response biases in preschool children's ratings of pain in hypothetical situations. Eur J Pain 2009;13(2):209-13.
10. Mangat AK, Oei JL, Chen K et al. A Review of Non-Pharmacological Treatments for Pain Management in Newborn Infants. Children (Basel) 2018;5(10).
11. Holsti L, Grunau RE. Considerations for using sucrose to reduce procedural pain in preterm infants. Pediatrics 2010;125(5):1042-7.
12. Collados-Gómez L, Ferrera-Camacho P et al. Randomised crossover trial showed that using breast milk or sucrose provided the same analgesic effect in preterm infants of at least 28 weeks. Acta Paediatr 2018;107(3):436-41.
13. Chen KL, Lindrea KB, Quah-Smith I et al. Magnetic noninvasive acupuncture for infant comfort (MAGNIFIC) – a single-blinded randomised controlled pilot trial. Acta Paediatr 2017;106(11):1780-6.
14. Kim D, Lee JY, Lee YJ et al. Comparative Effectiveness of Non-Pharmacological and Pharmacological Treatments for Non-Acute Lumbar Disc Herniation: A Multicenter, Pragmatic, Randomized Controlled, Parallel-Grouped Pilot Study. J Clin Med 2025;14(4).
15. Bellieni CV, Buonocore G, Nenci A et al. Sensorial saturation: an effective analgesic tool for heel-prick in preterm infants: a prospective randomized trial. Biol Neonate 2001;80(1):15-8.
16. Sabeti F, Mohammadpour M, Pouraboli B et al. Health Care Providers' Experiences of the Non-Pharmacological Pain and Anxiety Management and Its Barriers in the Pediatric Intensive Care Units. J Pediatr Nurs 2021;60:e110-e6.
17. Alavi A, Zargham A, Abdyzdan Z, Nmnbati M. The comparison of distraction and EMLA Cream effects on pain intensity due to intravenus Catheters in 5-12 years old thalassemic children. J Shahrekord University Med Sci 2005;7(3):9.
18. Nazemzadeh M, Bagherian S, Miri S et al. Non-pharmaceutical Methods of Anxiety and Pain Control in Children. Beyhagh 2015;17(1):31-9.
19. Bageriyan S, Borhani F, Abaszadeh A. The effect of non-pharmacologic pain management methods for venipuncture pain in school aged children in the center for thalassemia in the city of kerman. Nurs Midwifery J 2013;10(6).
20. Suleman SK, Yahya N, Nilsson S, Enskär K. Comparative efficacy of pharmacological and non-pharmacological interventions for mitigating pain and anxiety associated with venipuncture: a randomised controlled trial. BMJ Paediatr Open 2024;8(1).
21. Barkhordari AF, Sobhani G et al. The Effectiveness of Sedative and Non-pharmacological Premedication in Pediatric Anesthesia: A Review Article. J Ped Perspect 2019;7(12):10635-42.
22. Parvizi F, Alhani F, Aghebati N. The nurses’ problems in applying non-pharmacological pain management for children. Iran J Nurs Res 2008;3(9):85-92.
23. Byrd PJ, Gonzales I, Parsons V. Exploring barriers to pain management in newborn intensive care units: a pilot survey of NICU nurses. Adv Neonatal Care 2009;9(6):299-306.
24. Walker C. Use of art and play therapy in pediatric oncology. J Pediatr Oncol Nurs 1989;6(4):121-6.
25. Woollett N, Bandeira M, Hatcher A. Trauma-informed art and play therapy: Pilot study outcomes for children and mothers in domestic violence shelters in the United States and South Africa. Child Abuse Negl 2020;(107):104564.
26. Zempsky WT, Schechter NL. What's new in the management of pain in children. Pediatr Rev 2003;24(10):337-48.
27. Shahabi M, Kalani-Tehrani D, Eghbal M et al. Comparing the effects of EMLA ointment with a diversionary activity (music) on Vein Puncture pain at school-age children. Adv Nurs Midwifery 2007;17(56):13-20.
28. Hazinski MF. Nursing care of the critically ill child: Elsevier Health Sciences, 2012.
29. Namnabati M. The effect of distraction on pain from burn injuries at the Hospital for burn trauma, Isfahan. Res Med Sci 2002;7(1):67-9.
30. Anim-Boamah O, Ani-Amponsah M, Laari L, Aziato L. Pharmacological management of invasive procedural pain in children: Facilitators and barriers. Douleurs 2024;25(1):1-10.
31. Shaban M, Rasoolzadeh N, Mehran A, Moradalizadeh F. Study of two non-pharmacological methods, progressive muscle relaxation and music, on pain relief of cancerous patients. J Hayat 2006;12(3):63-72.